Meralgia paraesthetica refers to localised sensory symptoms of the outer thigh caused by compression of the lateral femoral cutaneous nerve. It is a mononeuropathy, meaning it only affects a single nerve.
Basic Anatomy
The lateral femoral cutaneous nerve originates from varying combinations of L1, L2 and L3 nerve roots. It comes from behind the psoas muscle, around the surface of the iliacus muscle and under the inguinal ligament onto the thigh, just medial and inferior to the anterior superior iliac spine (ASIS).
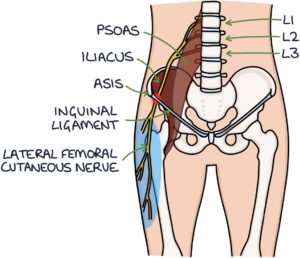
It supplies sensory innervation to the upper-outer thigh. Pressure, deformity or trauma to the nerve can occur at several places.
The lateral femoral cutaneous nerve only carries sensory signals. Therefore, there are no motor symptoms with meralgia paraesthetica.
Presentation
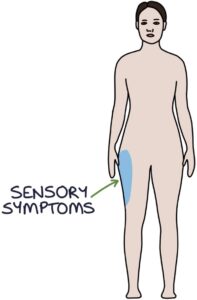
Patients present with abnormal sensations (dysaesthesia) and loss of sensation (anaesthesia) in the lateral femoral cutaneous nerve distribution. The skin of the upper-outer thigh is affected. Patients may describe symptoms of:
- Burning
- Numbness
- Pins and needles
- Cold sensation
There may also be localised hair loss.
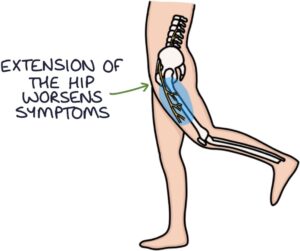
Symptoms are aggravated by walking or standing for a long duration and improve when sitting down.
Symptoms are often worse with extension of the hip on the affected side. This can be used to reproduce symptoms on examination.
Diagnosis
The diagnosis is mainly clinical, based on history and examination findings. Other investigations may be used to rule out other causes (e.g., nerve root compression in the spine or pelvic tumours compressing the nerve).
Management
Symptoms vary from mild and self-limiting to severe and persistent.
Management can be conservative, medical or surgical.
Conservative management involves:
- Rest
- Looser clothing (tight clothes such as belts may add pressure to the nerve)
- Weight loss (if appropriate)
- Physiotherapy
Medical management is based around analgesia if pain is a feature, such as:
- Paracetamol
- NSAIDs
- Neuropathic analgesia (e.g., amitriptyline, gabapentin, pregabalin or duloxetine)
- Local injections of steroids or local anaesthetics
Surgical management may involve:
- Decompression – removing pressure on the nerve
- Transection – cutting the nerve
- Resection – removing the nerve
Last updated August 2021
