An entire liver can be transplanted from a deceased donor to a recipient.
The liver has the ability to regenerate. It is possible to take a portion of the liver from a living donor, transplant it into a patient and have both regenerate to become two fully functioning organs. This is known as a living donor transplant.
It is also possible to split the liver of a deceased person into two and transplant the two parts into two patients and have them regenerate to function normally in both recipients. This is known as a split donation.
When the patient’s diseased liver is removed and the new liver placed in the same anatomical location, it is known as an orthotopic transplant. This translates as straight (ortho-) in place (-topic). This is in contrast to a heterotopic transplant, which involves adding the new organ away from the existing organs (e.g., adding a transplanted kidney in the lower abdomen without removing the native kidneys during a kidney transplant).
Indications
Indications for liver transplant can be split into two categories: acute liver failure or chronic liver failure. They may also be used in specific cases of hepatocellular carcinoma.
Acute liver failure usually requires an immediate liver transplant, and these patients are placed on the top of the transplant list. The most common causes are acute viral hepatitis and paracetamol overdose.
Chronic liver failure patients can wait longer for their liver transplant and are put on a standard transplant list. It is normal for it to take around 5 months for a liver to become available.
Factors Suggesting Unsuitability for Liver Transplantation
The British Society of Gastroenterologists provides guidelines on liver transplantation (2019), including when to refer and the contraindications.
Contraindications include:
- Significant co-morbidities (e.g., severe kidney, lung or heart disease)
- Current illicit drug use
- Continuing alcohol misuse (generally 6 months of abstinence is required)
- Untreated HIV
- Current or previous cancer (except certain liver cancers)
Surgery
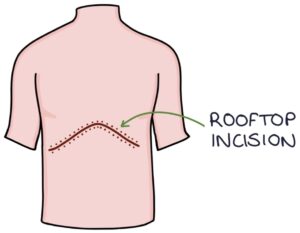
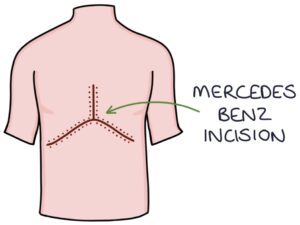
The liver transplant surgery is carried out in a specialist transplant centre. It involves a “rooftop” or “Mercedes Benz” incision along the lower costal margin for open surgery. The liver is mobilised away from the other tissues and excised. The new liver, biliary system and blood supply is then implanted and connected.
Post-Transplantation Care
Patients will require lifelong immunosuppression (e.g., steroids, azathioprine and tacrolimus) and careful monitoring of these drugs. They are required to follow lifestyle advice and require monitoring and treatment for complications:
- Avoid alcohol and smoking
- Treating opportunistic infections
- Monitoring for disease recurrence (i.e. of hepatitis or primary biliary cirrhosis)
- Monitoring for cancer as there is a significantly higher risk in immunosuppressed patients
Monitoring for evidence of transplant rejection:
- Abnormal LFTs
- Fatigue
- Fever
- Jaundice
Last updated May 2021
Now, head over to members.zerotofinals.com and test your knowledge of this content. Testing yourself helps identify what you missed and strengthens your understanding and retention.

