A diverticulum (plural diverticula) is a pouch or pocket in the bowel wall, usually ranging in size from 0.5 – 1cm.
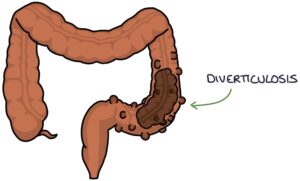
Diverticulosis refers to the presence of diverticula, without inflammation or infection. Diverticulosis may be referred to as diverticular disease when patients experience symptoms.
Diverticulitis refers to inflammation and infection of diverticula.
Pathophysiology
The wall of the large intestine contains a layer of muscle called the circular muscle. The points where this muscle layer is penetrated by blood vessels are areas of weakness. Increased pressure inside the lumen over time, can cause a gap to form in these areas of the circular muscle. These gaps allow the mucosa to herniate through the muscle layer and pouches to form (diverticula).
Diverticula do not form in the rectum, because it has an outer longitudinal muscle layer that completely surrounds the diameter of the rectum, adding extra support. In the rest of the colon, there are three longitudinal muscles that run along the colon, forming strips or ribbons called teniae coli. The teniae coli do not surround the entire diameter of the colon, and the areas that are not covered by teniae coli are vulnerable to the development of diverticula.
Diverticulosis
Diverticulosis is sometimes described in layman’s terms as “wear and tear of the bowel”. The most commonly affected section of the bowel is the sigmoid colon. However, it can affect the entire large intestine in some patients. Small bowel diverticula are also possible but much less common.
Diverticulosis is very common with increased age. Low fibre diets, obesity and the use of NSAIDs are risk factors. The use of NSAIDs increases the risk of diverticular haemorrhage.
It is often diagnosed incidentally on colonoscopy or CT scans. Treatment is not necessary where the patient is asymptomatic. However, advice regarding a high fibre diet and weight loss is appropriate.
Diverticulosis may cause lower left abdominal pain, constipation or rectal bleeding. Management is with increased fibre in the diet and bulk-forming laxatives (e.g., ispaghula husk). Stimulant laxatives (e.g., Senna) should be avoided. Surgery to remove the affected area may be required where there are significant symptoms.
Acute Diverticulitis
Diverticulitis refers to inflammation in the diverticula. Acute diverticulitis presents with:
- Pain and tenderness in the left iliac fossa / lower left abdomen
- Fever
- Diarrhoea
- Nausea and vomiting
- Rectal bleeding
- Palpable abdominal mass (if an abscess has formed)
- Raised inflammatory markers (e.g., CRP) and white blood cells
The NICE clinical knowledge summaries (updated January 2021) suggest management of uncomplicated diverticulitis in primary care with:
- Oral co-amoxiclav (at least 5 days)
- Analgesia (avoiding NSAIDs and opiates, if possible)
- Only taking clear liquids (avoiding solid food) until symptoms improve (usually 2-3 days)
- Follow-up within 2 days to review symptoms
Patients with severe pain or complications require admission to hospital. Hospital treatment involves management as with any patient with an acute abdomen or sepsis, including:
- Nil by mouth or clear fluids only
- IV antibiotics
- IV fluids
- Analgesia
- Urgent investigations (e.g., CT scan)
- Urgent surgery may be required for complications
Complications of acute diverticulitis are:
- Perforation
- Peritonitis
- Peridiverticular abscess
- Large haemorrhage requiring blood transfusions
- Fistula (e.g., between the colon and the bladder or vagina)
- Ileus / obstruction
Last updated May 2021
Now, head over to members.zerotofinals.com and test your knowledge of this content. Testing yourself helps identify what you missed and strengthens your understanding and retention.

