Facial nerve palsy refers to isolated dysfunction of the facial nerve and presents with unilateral facial weakness.
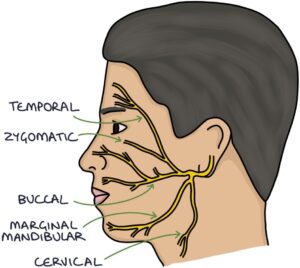
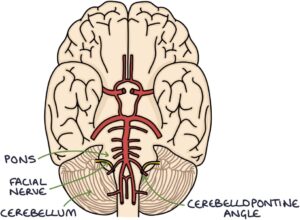
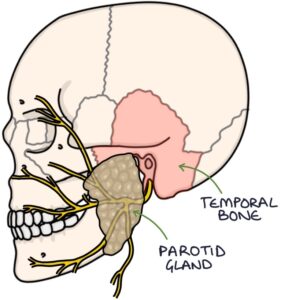
Facial Nerve Pathway
The facial nerve exits the brainstem at the cerebellopontine angle.
On its journey to the face, it passes through the temporal bone and parotid gland.
It then divides into five branches:
- Temporal
- Zygomatic
- Buccal
- Marginal mandibular
- Cervical
Facial Nerve Function
Motor function for:
- Facial expression
- Stapedius in the inner ear
- Posterior digastric, stylohyoid and platysma muscles
Sensory function for taste from the anterior 2/3 of the tongue.
Parasympathetic supply to the:
- Submandibular and sublingual salivary glands
- Lacrimal gland (stimulating tear production)
Upper Versus Lower Motor Neurone Lesion
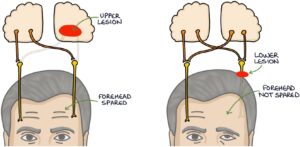
It is essential to distinguish between upper motor neurone and lower motor neurone facial nerve palsy. Patients with new-onset upper motor neurone facial nerve palsy need immediate management as a possible stroke. In contrast, patients with lower motor neurone facial nerve palsy can be managed less urgently.
Each side of the forehead has upper motor neurone innervation by both sides of the brain. However, each side of the forehead only has lower motor neurone innervation from one side of the brain.
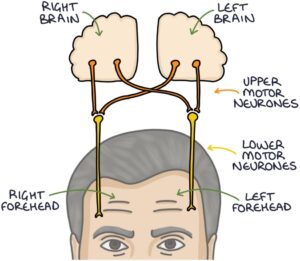
The forehead will be spared in an upper motor neurone lesion so the patient can move their forehead on the affected side. In a lower motor neurone lesion, the forehead is not spared, and the patient cannot move their forehead on the affected side.
Upper Motor Neurone Lesions
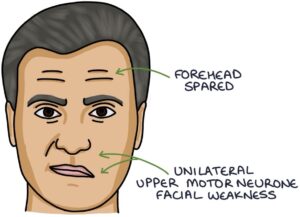
Unilateral upper motor neurone lesions occur in:
- Cerebrovascular accidents (strokes)
- Tumours
Bilateral upper motor neurone lesions are rare. They may occur in:
- Pseudobulbar palsies
- Motor neurone disease
Bell’s Palsy
Bell’s palsy is a relatively common condition. It is idiopathic, meaning there is no apparent cause. It presents with a unilateral lower motor neurone facial nerve palsy.
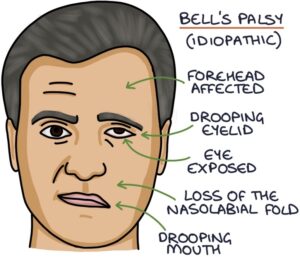
Most patients fully recover over several weeks, but recovery may take up to 12 months. A third are left with some residual weakness.
If patients present within 72 hours of developing symptoms, NICE clinical knowledge summaries (updated 2023) recommend considering prednisolone as treatment, either:
- 50mg for 10 days
- 60mg for 5 days followed by a 5-day reducing regime, dropping the dose by 10mg per day
Patients also require lubricating eye drops to prevent the eye from drying out and being damaged. If they develop pain in the eye, they need an ophthalmology review for exposure keratopathy. The eye can be taped closed at night.
Ramsay-Hunt Syndrome
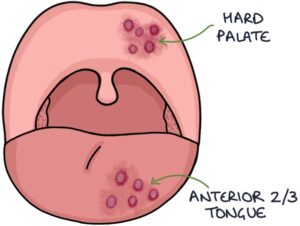
Ramsay-Hunt syndrome is caused by the varicella zoster virus (VZV). It presents as a unilateral lower motor neurone facial nerve palsy. Patients stereotypically have a painful and tender vesicular rash in the ear canal, pinna and around the ear on the affected side.
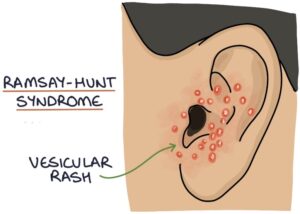
This rash can extend to the anterior two-thirds of the tongue and hard palate.
Treatment is with aciclovir and prednisolone. Patients also require lubricating eye drops.
TOM TIP: Ramsay-Hunt syndrome is popular in MCQ exams. Look out for the patient with facial nerve palsy and a vesicular rash around their ear.
Other Causes of Lower Motor Neurone Facial Nerve Palsy
Infections:
- Otitis media
- Otitis externa
- HIV
- Lyme disease
Systemic diseases:
- Diabetes
- Sarcoidosis
- Leukaemia
- Multiple sclerosis
- Guillain–Barré
Tumours:
- Acoustic neuroma
- Parotid tumour
- Cholesteatoma
Trauma:
- Direct nerve trauma
- Surgery
- Base of skull fractures
Last updated March 2025
Now, head over to members.zerotofinals.com and test your knowledge of this content. Testing yourself helps identify what you missed and strengthens your understanding and retention.