A coronary artery bypass graft (CABG) procedure involves using a graft blood vessel taken from elsewhere in the body (usually the saphenous vein) to bypass a blockage in a coronary artery. Depending on the affected areas, this may involve one, two, three or even four bypass grafts.
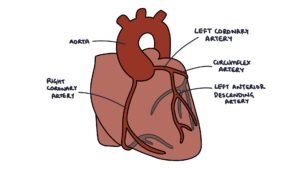
Coronary Anatomy
The left coronary artery (LCA) becomes the circumflex and left anterior descending (LAD) arteries.
The right coronary artery (RCA) curves around the right side and under the heart and supplies the:
- Right atrium
- Right ventricle
- Inferior aspect of the left ventricle
- Posterior septal area
The circumflex artery curves around the top, left and back of the heart and supplies the:
- Left atrium
- Posterior aspect of the left ventricle
The left anterior descending (LAD) travels down the middle of the heart and supplies the:
- Anterior aspect of the left ventricle
- Anterior aspect of septum
Atherosclerosis
Athero- refers to soft or porridge-like and -sclerosis refers to hardening. Atherosclerosis is a combination of atheromas (fatty deposits in the artery walls) and sclerosis (the process of hardening or stiffening of the blood vessel walls). Atherosclerosis affects the medium and large arteries. It is caused by chronic inflammation and activation of the immune system in the artery wall. Lipids are deposited in the artery wall, followed by the development of fibrous atheromatous plaques.
These plaques cause:
- Stiffening of the artery walls, leading to hypertension (raised blood pressure) and strain on the heart (whilst trying to pump blood against increased resistance)
- Stenosis, leading to reduced blood flow (e.g., in angina)
- Plaque rupture, resulting in a thrombus that can block a distal vessel and cause ischaemia (e.g., in acute coronary syndrome)

Atherosclerosis Risk Factors
It is important to break these down into modifiable and non-modifiable risk factors. We cannot do anything about non-modifiable risk factors, but we can do something about modifiable ones.
Non-modifiable risk factors:
- Older age
- Family history
- Male
Modifiable risk factors:
- Smoking
- Alcohol consumption
- Poor diet (high in sugar and trans-fat and low in fruit, vegetables and omega 3s)
- Low exercise / sedentary lifestyle
- Obesity
- Poor sleep
- Stress
Medical Co-Morbidities
Medical co-morbidities increase the risk of atherosclerosis and should be carefully managed to minimise the risk:
- Diabetes
- Hypertension
- Chronic kidney disease
- Inflammatory conditions such as rheumatoid arthritis
- Atypical antipsychotic medications
TOM TIP: Think about risk factors when taking a history from someone with suspected atherosclerotic disease (such as someone presenting with intermittent claudication). Ask about their exercise, diet, past medical history, family history, occupation, smoking, alcohol intake and medications. This will help you perform well in exams and when presenting to seniors.
Complications of Atherosclerosis
- Angina
- Myocardial infarction
- Transient ischaemic attack
- Stroke
- Peripheral arterial disease
- Chronic mesenteric ischaemia
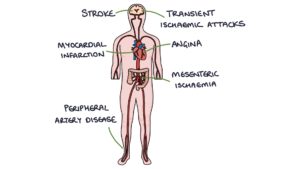
TOM TIP: Patients with one type of arterial disease are likely to have others. When a patient has symptoms of one type of arterial disease (e.g., intermittent claudication), consider the risk of others (e.g., coronary artery disease). Erectile dysfunction can often be the first indication of arterial disease and should prompt you to consider checking the lipid profile, blood pressure and Q-risk score (which is the percentage risk that a patient will have a stroke or myocardial infarction in the next 10 years).
Coronary Artery Disease
Narrowing (stenosis) of the coronary arteries due to atherosclerosis may be asymptomatic, or present with:
- Angina (stable or unstable)
- Myocardial infarction
The options for management are:
- Medical management (secondary prevention with statins, aspirin, beta-blockers and ACE inhibitors)
- Percutaneous coronary intervention (PCI) with coronary angioplasty
- Coronary artery bypass graft
Cardiopulmonary Bypass
The bypass machine takes blood from the vena cava or right atrium, pumps it through a machine that adds oxygen and removes carbon dioxide from the blood, then pumps it back into the ascending aorta. This way, blood bypasses the heart and lungs and is artificially oxygenated. Heparin is used to prevent blood clotting. The clinical perfusionist is responsible for operating and monitoring the cardiopulmonary bypass equipment.
Cardioplegia
During a coronary artery bypass graft procedure, the heart needs to be still. Causing the heart to stop beating is called cardioplegia. The heart is only stopped after the cardiopulmonary bypass is up and running. A high potassium solution is delivered into the coronary circulation, causing the heart to stop. Once the surgery is complete, cardioplegia is stopped and the heart will spontaneously start beating. Cardioversion or temporary pacing may be used to treat arrhythmias that occur.
Coronary Artery Bypass Grafts
A separate blood vessel needs to be obtained to create a bypass. This blood vessel is called a graft. The three main options for graft vessels are:
- Saphenous vein (harvested from the inner leg)
- Internal thoracic artery, also known as the internal mammary artery
- Radial artery
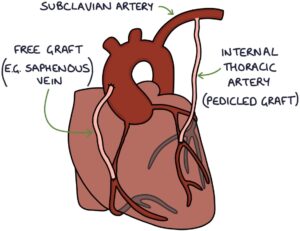
The internal thoracic artery is a branch of the subclavian artery. When the internal thoracic artery is used in a CABG, the proximal end may be left attached to the subclavian artery. The distal end is separated from any connections and then joined to the left anterior descending artery. As a result, blood flows from the subclavian artery, through the internal thoracic artery and into the left anterior descending artery. Leaving it proximally attached to the original site, whilst changing where it supplies, is described as a pedicled graft. The internal thoracic artery can also be used as a free graft if required.
A free graft refers to a section of blood vessel that is entirely separated from its original connections, before being reattached in a new site for the bypass. During a coronary artery bypass procedure, the graft vessel is attached directly to the ascending aorta, with the other end attached to the coronary artery, distal to the stenosis (bypassing the diseased portion of the artery). Blood flows from the ascending aorta, through the graft and into the coronary artery.
Vein grafts (i.e., from the saphenous vein) have a tendency to become stenosed (narrowed) over time in a process called intimal hyperplasia. The tunica intima layer in the vessel becomes thickened, mostly due to increased pressure. Arterial grafts (e.g., radial or internal thoracic) are less affected by this, so tend to make better grafts.
Recovery
After cardiothoracic surgery, patients have careful monitoring and supportive care in the intensive care unit. They are usually discharged after about a week. There is a slow recovery period with a gradual increase in activity. In straightforward cases, patients make a full recovery and resume full normal activities after 3 months.
Complications
The two most serious and notable complications are:
- Death (2-3% in straightforward cases)
- Stroke (1-5% in straightforward cases)
Other complications:
- Infection
- Acute kidney injury
- Cognitive impairment
- Myocardial infarction
- Atrial fibrillation
Last updated May 2021
Now, head over to members.zerotofinals.com and test your knowledge of this content. Testing yourself helps identify what you missed and strengthens your understanding and retention.