Meanings of Prefixes and Suffixes
- Baso: foundation
- Blasts: immature cells
- Cyte: cell
- Eosin: red coloured
- Haemo: blood
- Karyo: nucleus
- Kine: motion
- Lympho: lymphatic system
- Lysis: broken down
- Macro: large
- Mega: large
- Mono: single
- Myelo: bone marrow
- Neutro: neutral
- Phage: eat
- Phil: attraction
- Pluri: multiple
- Poietic: creative
- Potent: potential
- Pro: moving forward
- Reticulo: net like
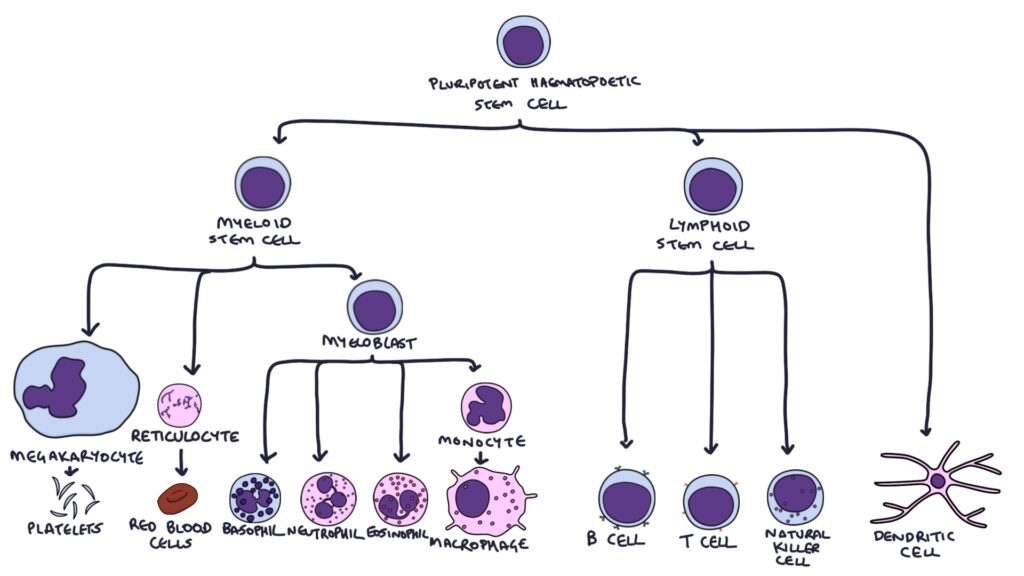
Pluripotent Haematopoietic Stem Cell
These are undifferentiated cells that have the potential to become a variety of blood cells. They initially become:
- Myeloid Stem Cells
- Lymphoid Stem Cells
- Dendritic Cells (via various intermediate cells)
Myeloid Stem Cells
Myeloid stem cells become:
- Megakaryocytes that produce platelets
- Reticulocytes become:
- Red Blood Cells (RBCs)
- Promyelocytes become:
- Monocytes – Macrophages
- Neutrophils
- Eosinophils
- Mast Cells
- Basophils
Lymphoid Stem Cells
Lymphoid Stem Cells travel to the thymus gland and differentiate into:
- B lymphocytes (B cells) (mature in the bone marrow) that differentiate into:
- Plasma Cells
- Memory B Cells
- T lymphocytes (T cells) (mature in the thymus) that differentiate into:
- CD4 cells (T helper cells)
- CD8 cells (Cytotoxic T Cells)
- Natural Killer Cells
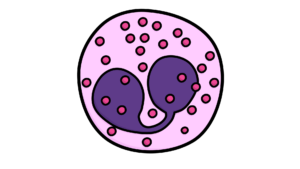
Megakaryocytes
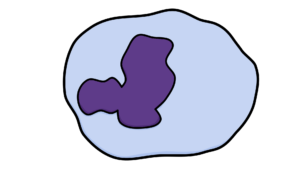
- Large cells
- Big lobulated nucleus
- Produce platelets
- Platelets are essential for blood clotting
Reticulocytes

- Immature red blood cells
- Remnant RNA material called reticulum in cytoplasm
- Released from bone marrow
- Normally 1% of red blood cells are reticulocytes
- Higher percentage indicates rapid turnover of blood, such as in:
- Acute blood loss
- Haemolysis
- Loose their reticulum after a few days – becoming:
Red Blood Cells (RBCs)

- RBCs contain large quantities of haemoglobin, and carry oxygen from the lungs to the tissues
- They survive about 3 months
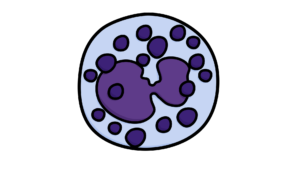
Macrophages
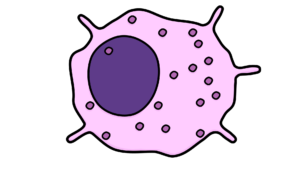
- Monocytes circulate the blood stream
- Enter tissues and differentiate into macrophages
- Live in most tissues in the body
- Have “Toll-Like Receptors“
- Recognise “Pathogen-associated molecular patterns” (PAMPs)
- Kill pathogens and abnormal cells by phagocytosis
- Release cytokines that initiate the inflammatory response
- Activate the other cells of the immune system
Neutrophils
- Circulate through the blood and lymphatic system
- Migrate to areas of inflammation
- Kill pathogens and abnormal cells by phagocytosis
Eosinophils
- Important in responding to parasites
- They normally sit waiting in tissues
- Contain granules with:
- Proinflammatory cytokines
- Chemicals toxic to pathogens, such as “major basic protein“
- They have two functions:
- Exocytosis of their granules
- Phagocytosis (but less than neutrophils and macrophages)
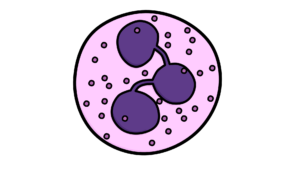
Mast Cells and Basophils
- Mast cells are fixed in place in tissues
- Basophils circulate through the blood
- Contain cytoplasmic granules
- Degranulation releases pro-inflammatory cytokines
B Lymphocytes
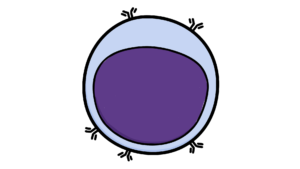
- Also called B cells
- Mature in the bone marrow
- Cell surface lined with antibodies
- Each B cell has a specific type of antibody for a specific antigen
- There are millions of different possible antibodies and therefore millions of different specific B cells
- B cells can only recognise antigens that match their antibodies
- Once activated B cells become either:
- Plasma cell – secrete antibodies (also called immunoglobulins)
- Memory B cell – await a later infection with the same pathogen
T Lymphocytes
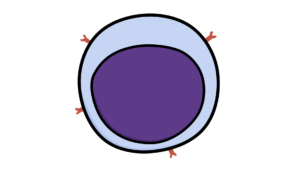
- Also called T cells
- Pro-thymocytes leave the bone marrow and travel to the thymus gland
- Mature in the thymus gland into T cells
- Cell surface lined with T-cell receptors
- Each T cell has a specific type of T-cell Receptor (TcR) for a specific antigen
- CD4 cells have CD4 TcRs that recognise MHC class 2 receptors
- CD8 cells have CD8 TcRs that recognise MHC class 1 receptors
- CD4 cells become T-helper cells when activated
- T helper cells help other cells become activated, including CD8 cells
- CD8 cells become cytotoxic T cells when activated
- Cytotoxic T cells destroy infected cells via
- Granule exocytosis causing destruction of the cell
- Activating the Fas pathway causing cell apoptosis
Natural Killer Cells
- Activated by cytokines from macrophages and interferons
- Recognise infected or abnormal (e.g. cancerous) cells
- Destroy these cells by cytokines
- Release IFN-γ that activates macrophages
Dendritic Cells

- Originate from several cell lines
- Specialist dendritic cells found in the skin are called Langerhans cells
- Take up antigens, process them and display them on their cell surface
- Have both MHC class I and class II molecules
- Act as messengers, taking antigens from infected tissues to lymph nodes to activate T cells
