The renin-angiotensin-aldosterone system (RAAS) is central in the regulation of:
- Blood pressure
- Electrolyte balance
- Blood vessel and heart remodelling
Renin-Angiotensin-Aldosterone System
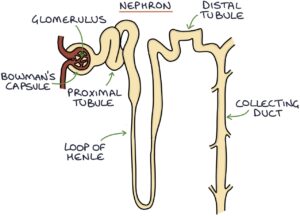
Inside the kidneys, many tiny structures called nephrons filter the blood and produce urine. The basic structures of the nephron are the glomerulus, proximal tubule, loop of Henle, distal tubule and collecting duct.
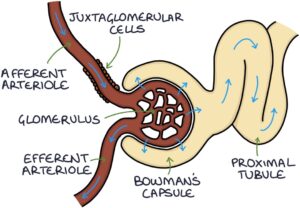
At the start of the nephron is the glomerulus. The afferent arterioles bring blood into the glomerulus, and the efferent arterioles drain blood out of the glomerulus. Fluid filters from the blood in the glomerulus into Bowman’s capsule, the first part of the nephron. The filtered fluid is called filtrate. This fluid travels along the nephron, where various chemicals are secreted and reabsorbed before it eventually drains through the collecting ducts and out of the kidney as urine.
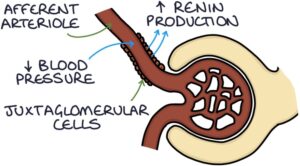
The juxtaglomerular cells are found at the afferent arterioles. They sense the blood pressure in the afferent arterioles and secrete an enzyme called renin, depending on the pressure. They secrete more renin in response to low blood pressure and less renin in response to high blood pressure.
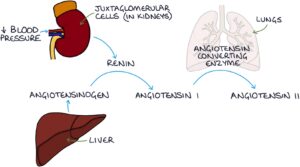
The liver produces a protein called angiotensinogen. Renin acts to convert angiotensinogen into angiotensin I. Angiotensin I converts to angiotensin II in the lungs with the help of angiotensin-converting enzyme (ACE).
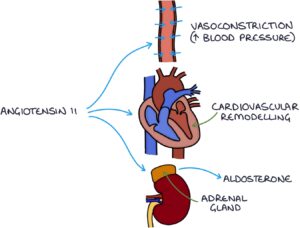
Angiotensin II has three main effects. It stimulates:
- Vasoconstriction (acting on the blood vessels directly)
- Hypertrophy (thickening) and remodelling of the heart and blood vessels
- Aldosterone release by the adrenal glands
Angiotensin II acts on blood vessels, causing vasoconstriction. Vasoconstriction occurs when the smooth muscle of the blood vessel walls contracts, narrowing the lumen of the blood vessels and increasing the resistance and pressure within them. In this way, angiotensin II directly acts on blood vessels to increase blood pressure.
Long-term, angiotensin II stimulates hypertrophy (thickening) of the heart muscle (myocardium) and vascular smooth muscle, causing cardiac remodelling and thickening of the blood vessel walls.
Angiotensin II stimulates the adrenal glands to release aldosterone.
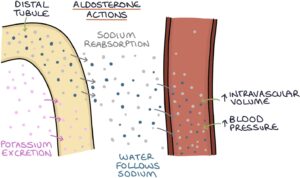
Aldosterone is a mineralocorticoid steroid hormone. It acts on the nephrons in the kidneys to:
- Increase sodium reabsorption from the distal tubule
- Increase potassium secretion from the distal tubule
- Increase hydrogen secretion from the collecting ducts
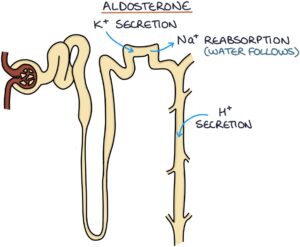
When sodium is reabsorbed from the filtrate back into the blood, water follows it by osmosis. This leads to:
- More fluid retained in the body
- Increased intravascular volume (that volume of fluid inside the blood vessels)
- Increased blood pressure (due to a greater volume of fluid inside the blood vessels)
Fludrocortisone is a mineralocorticoid medication used to replace aldosterone in patients with adrenal insufficiency. It is also used to treat postural hypotension by increasing and maintaining blood pressure in patients with low blood pressure on standing.
Hyperaldosteronism
Hyperaldosteronism refers to raised aldosterone. Hyperaldosteronism may be present in 5-10% of patients with hypertension (high blood pressure). Hypertension is the crucial presenting feature, and many patients are otherwise asymptomatic. It may cause non-specific symptoms such as headaches, muscle weakness and fatigue.
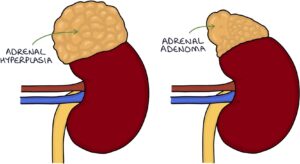
Primary hyperaldosteronism is when the adrenal glands are directly responsible for producing too much aldosterone. High blood pressure is sensed by the juxtaglomerular cells in the kidneys, and they respond by reducing the production of renin. Therefore, the serum renin will be low, as it is suppressed by the high blood pressure. The adrenals may produce too much aldosterone for several possible reasons:
- An adrenal adenoma secreting aldosterone (Conn’s syndrome)
- Bilateral adrenal hyperplasia (enlargement and over-functioning of the adrenals)
- Familial hyperaldosteronism (rare)
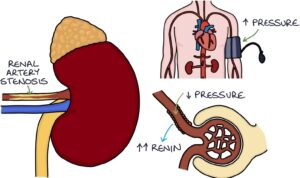
Secondary hyperaldosteronism is caused by excess renin stimulating the release of excess aldosterone. Excess renin is released due to disproportionately lower blood pressure in the kidneys. The blood pressure in the limbs may be normal or high, but the blood pressure that reaches the juxtaglomerular cells inside the kidneys is low. This may be due to:
- Renal artery stenosis
- Heart failure
- Liver cirrhosis and ascites
Renal artery stenosis refers to narrowing of the renal arteries supplying the kidneys, usually due to atherosclerosis, similar to coronary artery narrowing in angina. The narrow entry to the kidney results in a lower blood pressure inside the kidney, even when the systemic blood pressure is high. The juxtaglomerular cells think the entire body has a low blood pressure problem and responds by excreting lots of renin, which in turn increases the aldosterone level.
A aldosterone-to-renin ratio blood test can be used to screen for primary hyperaldosteronism.
|
Aldosterone |
Renin |
Aldosterone-To-Renin Ratio |
|
|
Primary Hyperaldosteronism |
High |
Low |
High |
|
Secondary Hyperaldosteronism |
High |
High |
Normal |
Medications that Inhibit the Renin-Angiotensin-Aldosterone System
Three common classes of medications are used to inhibit the renin-angiotensin-aldosterone system (RAAS):
- ACE inhibitors (e.g., ramipril and lisinopril)
- Angiotensin II receptor blockers (e.g., candesartan and losartan)
- Aldosterone antagonists (e.g., spironolactone and eplerenone)
These medications are used to treat various conditions, notably:
- Hypertension (high blood pressure)
- Heart failure
- Chronic kidney disease
ACE inhibitors (e.g., ramipril and lisinopril) work by blocking the action of angiotensin-converting enzyme (ACE). This stops angiotensin I from being converted to angiotensin II, lowering the amount of angiotensin II in the body. Lower angiotensin II results in less vasoconstriction, lower aldosterone, and less cardiac remodelling over the longer term. This means lower blood pressure, less fluid retention and a healthier heart and cardiovascular system.
Angiotensin II receptor blockers (e.g., candesartan and losartan) work by blocking angiotensin II receptors, blocking the effects of angiotensin II. Like ACE inhibitors, they result in less vasoconstriction, lower aldosterone, and less cardiac remodelling over the longer term.
Aldosterone antagonists work by blocking the receptors that aldosterone acts on, inhibiting the effects of aldosterone. They result in less sodium reabsorption and less potassium secretion in the distal tubules in the kidneys. More sodium is excreted from the body in the urine. Water follows the sodium by osmosis and is excreted in the urine, resulting in diuresis (increased urine production). Less potassium is excreted in the urine, meaning it is retained in the body. Therefore, they are known as potassium-sparing diuretics. Hyperkalaemia (high potassium) is a potential side effect.
Last updated January 2025
Now, head over to members.zerotofinals.com and test your knowledge of this content. Testing yourself helps identify what you missed and strengthens your understanding and retention.

