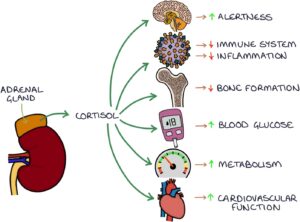
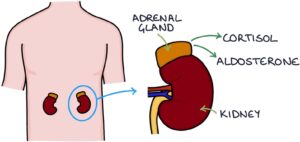
Cortisol is a glucocorticoid steroid hormone secreted by the two adrenal glands. The adrenal glands are found above the kidneys in the abdomen. Cortisol is a stress hormone released in response to stress and helps the body cope. It has several actions within the body:
- Increases alertness
- Inhibits the immune system and reduces inflammation
- Inhibits bone formation
- Raises blood glucose
- Increases metabolism
- Supports cardiovascular function (heart rate, blood pressure and cardiac output)
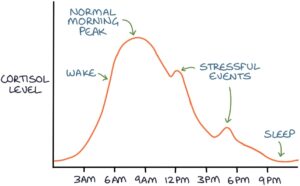
Cortisol is released in pulses throughout the day and in response to stressful stimuli. It has diurnal variation, meaning it is high and low at different times of the day. Cortisol typically peaks in the early morning, triggering the person to wake up and get going, and is at its lowest late in the evening, helping the person to relax and fall asleep.
Glucocorticoids and Mineralocorticoids
There are two types of steroid hormone produced by the adrenal glands:
- Glucocorticoid (cortisol)
- Mineralocorticoid (aldosterone)
Glucocorticoids (e.g., cortisol) have the actions listed above. They help the body cope with stress, regulate the immune system and reduce inflammation. Medications that act as glucocorticoids include:
- Prednisolone
- Hydrocortisone
- Dexamethasone
Mineralocorticoids (e.g., aldosterone) help regulate the balance of electrolytes and blood pressure. They act on the nephrons in the kidneys to:
- Increase sodium reabsorption from the distal tubule
- Increase potassium secretion from the distal tubule
- Increase hydrogen secretion from the collecting ducts
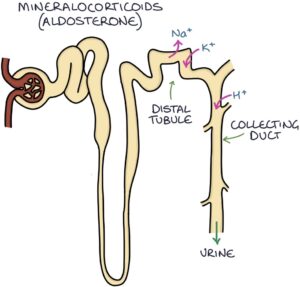
When sodium is reabsorbed in the kidneys, water follows it by osmosis. This leads to increased intravascular volume and, subsequently, blood pressure.
Fludrocortisone is a mineralocorticoid medication used to replace aldosterone in patients with adrenal insufficiency. It is also used to treat postural hypotension by increasing and maintaining blood pressure in patients who develop low blood pressure while standing.
Cortisol Control
Cortisol is controlled by two structures in the brain called the hypothalamus and the pituitary gland, specifically the anterior part of the pituitary.
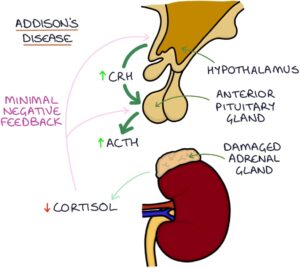
The hypothalamus releases corticotropin-releasing hormone (CRH). CRH stimulates the anterior pituitary to release adrenocorticotropic hormone (ACTH). ACTH stimulates the adrenal glands to release cortisol.
Cortisol travels to the body tissues to carry out its effects. It also travels to the brain and has a suppressing effect on the hypothalamus and the pituitary. This is called negative feedback. Too much cortisol suppresses the release of CRH and ACTH, helping to keep cortisol levels within normal limits.
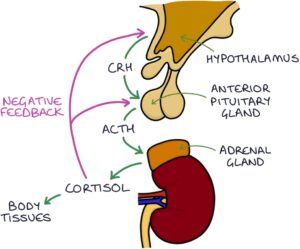
When the cortisol level gets too high, it suppresses the secretion of CRH and ACTH. Lower CRH and ACTH result in less adrenal gland stimulation and less cortisol secretion, returning the cortisol levels to normal.
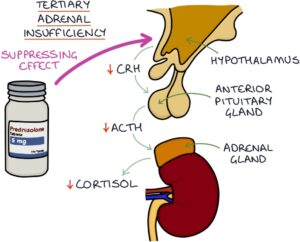
An excellent example of negative feedback in action is when we give patients glucocorticoid steroid medications, such as prednisolone, for an extended period. The prednisolone acts on the hypothalamus and pituitary like cortisol, suppressing the release of CRH and ACTH. There are very low levels of CRH and ACTH, with very little stimulation of the adrenal glands. The adrenals stop producing cortisol.
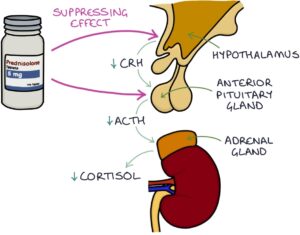
In this way, extended use of exogenous steroids (steroids originating outside the body), such as prednisolone, shuts down the production of endogenous steroids (steroids originating inside the body). The body cannot function without glucocorticoids. Since the body is not producing steroids naturally, the patient becomes entirely dependent on taking the steroids every day. Suddenly stopping the steroids can be dangerous, leading to a life-threatening adrenal crisis with insufficient glucocorticoids in the body. Steroid medications must be slowly reduced to give the body time to restart natural glucocorticoid production.
When cortisol levels get too low, CRH and ACTH are less suppressed, resulting in more CRH and ACTH secretion, more adrenal stimulation, and more cortisol secretion, bringing the levels back up.
Cushing’s Syndrome
Excessive cortisol (or taking long-term glucocorticoid medications) leads to Cushing’s syndrome. You can remember the causes of Cushing’s syndrome with the “CAPE” mnemonic:
- C – Cushing’s disease (a pituitary adenoma releasing excessive ACTH)
- A – Adrenal adenoma (an adrenal tumour secreting excess cortisol)
- P – Paraneoplastic syndrome
- E – Exogenous steroids (patients taking long-term corticosteroids)
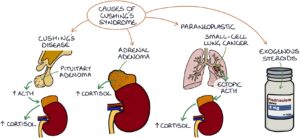
TOM TIP: Cushing’s disease refers to a specific scenario where a pituitary adenoma (a hormone-secreting tumour) releases excessive ACTH. High ACTH stimulates the release of excessive cortisol by the adrenal glands. Cushing’s disease causes Cushing’s syndrome. The distinction between Cushing’s disease and Cushing’s syndrome is worth noting.
Cushing’s syndrome results in typical symptoms and signs of:
- Round face (known as a “moon face”)
- Central obesity
- Abdominal striae (stretch marks)
- Enlarged fat pad on the upper back (known as a “buffalo hump”)
- Proximal limb muscle wasting (with difficulty standing from a sitting position without using their arms)
- Male pattern facial hair in women (hirsutism)
- Easy bruising and poor skin healing
- Insomnia
- Anxiety and depression
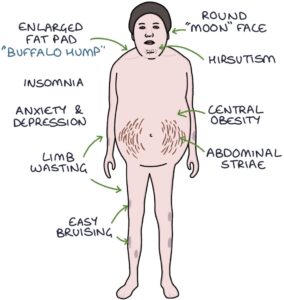
Metabolic effects of too much cortisol include:
- Hypertension
- Cardiac hypertrophy
- Type 2 diabetes
- Dyslipidaemia (raised cholesterol and triglycerides)
- Osteoporosis
Adrenal Insufficiency
Inadequate cortisol is referred to as adrenal insufficiency. Adrenal insufficiency is potentially life-threatening.
Adrenal insufficiency presents with potential symptoms of:
- Fatigue
- Muscle weakness
- Muscle cramps
- Dizziness and fainting
- Thirst and craving salt
- Weight loss
- Abdominal pain
- Depression
- Reduced libido

The signs of adrenal insufficiency are:
- Bronze hyperpigmentation of the skin, particularly in the skin creases (palms), scars, lips and buccal mucosa
- Hypotension (particularly postural hypotension – with a drop of more than 20 mmHg on standing)
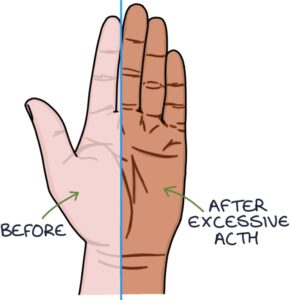
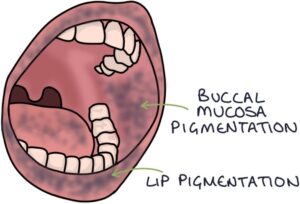
TOM TIP: A high level of ACTH causes skin pigmentation by stimulating melanocytes in the skin to produce melanin, similar to melanocyte-stimulating hormone. Increased skin pigmentation is a sign of Cushing’s disease (where excess ACTH comes from a pituitary adenoma) and primary adrenal insufficiency (where there is inadequate cortisol from the adrenals with a lack of negative feedback to the pituitary).
Addison’s disease refers specifically to when the adrenal glands have been damaged, resulting in reduced cortisol and aldosterone secretion. This is called primary adrenal insufficiency. It is primary, as the problem is with the direct source of cortisol (the adrenal glands). The most common cause is autoimmune, where the immune system gets confused and inappropriately attacks and damages the adrenal glands. Low cortisol means reduced negative feedback on the hypothalamus and pituitary, leading to increased CRH and ACTH.
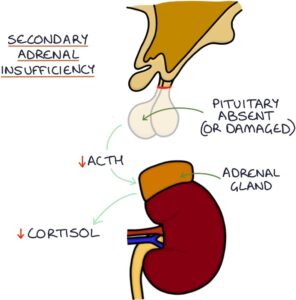
Secondary adrenal insufficiency occurs when inadequate ACTH is produced by the pituitary gland (e.g., after surgical removal of the pituitary). Inadequate ACTH means low adrenal stimulation and insufficient cortisol release. It is secondary, as the problem is one step back from the adrenal glands.
Tertiary adrenal insufficiency occurs when the hypothalamus produces inadequate CRH, usually due to suppression by exogenous glucocorticoids (e.g., long-term treatment with prednisolone). Inadequate CRH and ACTH mean low adrenal stimulation and reduced cortisol secretion. It is tertiary, as the problem is two steps back from the adrenal glands.
Adrenal crisis, also known as Addisonian crisis, describes an acute presentation of severe adrenal insufficiency, where the absence of steroid hormones leads to a life-threatening emergency. It presents with:
- Reduced consciousness
- Hypotension (low blood pressure)
- Hypoglycaemia (low blood glucose)
- Hyponatraemia (low sodium) and hyperkalaemia (high potassium)
Testing
Cortisol and ACTH can be tested on a blood sample. A single cortisol result is unreliable, as the levels fluctuate significantly throughout the day. There should be a relatively reliable increase in cortisol in the morning. Therefore, taking an early morning cortisol (taken at 8-9 am) may be used as an initial test for adrenal insufficiency. In adrenal insufficiency, the early morning cortisol may be lower than expected.
Dynamic tests are required to diagnose adrenal insufficiency or Cushing’s syndrome. These involve giving a hormone and seeing how the body responds.
Short Synacthen Test
The short Synacthen test (or ACTH stimulation test) is used to diagnose primary adrenal insufficiency. It involves giving a dose of Synacthen (synthetic ACTH) and monitoring the blood cortisol before and at 30 and 60 minutes after the dose. Synthetic ACTH stimulates healthy adrenal glands to produce cortisol. A failure of the cortisol levels to at least double indicates primary adrenal insufficiency. The damaged and dysfunctional adrenal glands fail to respond to the ACTH.

Dexamethasone Suppression Test
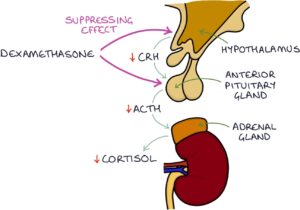
The dexamethasone suppression test is used to diagnose Cushing’s syndrome. It involves giving a dose of dexamethasone, a synthetic glucocorticoid, and monitoring what happens to the cortisol level using blood tests. Dexamethasone causes negative feedback on the hypothalamus and pituitary, reducing the CRH and ACTH output. Lower CRH and ACTH levels reduce cortisol production by the adrenal glands. A normal response to dexamethasone is suppressed cortisol.
In patients with an adrenal adenoma, dexamethasone will have no effect on the amount of cortisol released. The tumour is secreting large amounts of cortisol without requiring any stimulation by ACTH. In fact, ACTH will be suppressed by the high cortisol level before dexamethasone is even given.
In patients with ectopic ACTH (e.g., small cell lung cancer secreting ACTH), dexamethasone will have no effect on how much cortisol is released. It will suppress ACTH release by the pituitary, but there will still be lots of ACTH from elsewhere (e.g., the lung tumour) stimulating the adrenal glands to release cortisol.
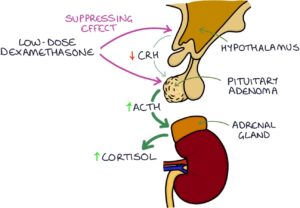
The initial test is the low-dose dexamethasone suppression test. A low dose of dexamethasone is given. In patients with a pituitary adenoma, a low dose of dexamethasone is not able to suppress the ACTH release. Therefore, cortisol will not be suppressed.
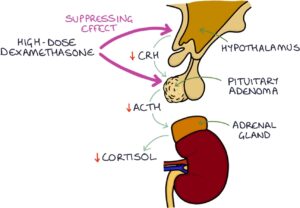
Further testing involves the high-dose dexamethasone suppression test. In patients with a pituitary adenoma, a high dose of dexamethasone is enough to suppress ACTH, resulting in lower cortisol.
|
Baseline ACTH |
Low Dose Test (Cortisol Result) |
High Dose Test (Cortisol Result) |
|
|
Normal |
Normal |
Low |
Low |
|
Adrenal Adenoma |
Low |
Not Suppressed |
Not Suppressed |
|
Pituitary Adenoma |
High |
Not Suppressed |
Low |
|
Ectopic ACTH |
High |
Not Suppressed |
Not Suppressed |
Last updated July 2024
Now, head over to members.zerotofinals.com and test your knowledge of this content. Testing yourself helps identify what you missed and strengthens your understanding and retention.