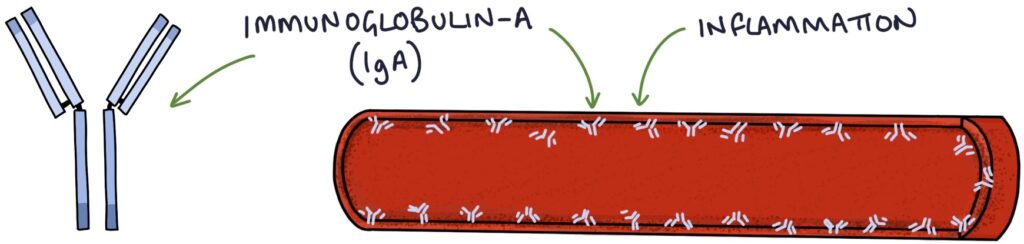
Henoch-Schonlein Purpura (HSP) is an IgA vasculitis that presents with a purpuric rash affecting the lower limbs and buttocks in children. Inflammation occurs in the affected organs due to IgA deposits in the blood vessels.
It affects the skin, kidneys and gastro-intestinal tract. The condition is often triggered by an upper airway infection or gastroenteritis. It is most common in children under the age of 10 years.
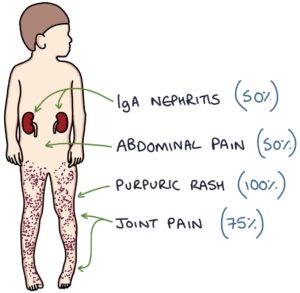
The four classic features are:
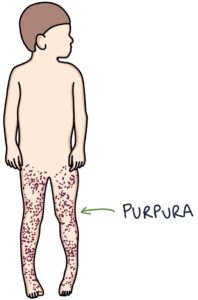
- Purpura (100%),
- Joint pain (75%),
- Abdominal pain (50%)
- Renal involvement (50%)
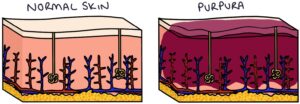
The rash is caused by inflammation and leaking of blood from small blood vessels under the skin, forming purpura. Purpura are red-purple lumps under the skin containing blood.
Features
Purpura are seen in practically 100% of patients with HSP. They are red-purple in colour and are palpable under the skin. Typically they start on the legs and spread to the buttocks. They can also affect the trunk and arms. In severe cases, skin ulceration and necrosis can develop.
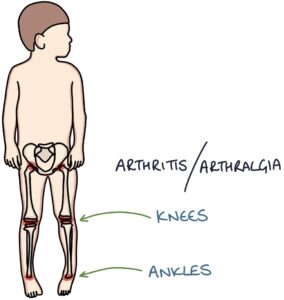
75% of patients with HSP develop arthralgia or arthritis, mostly affecting the knees and ankles. The joints can become swollen and painful, with a reduced range of movement.
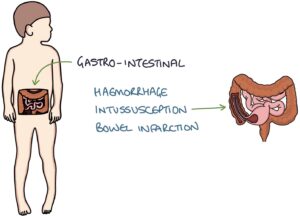
Abdominal pain is indicative of gastrointestinal involvement. This affects around 50% of patients with HSP. In severe cases, it can lead to gastrointestinal haemorrhage, intussusception and bowel infarction.
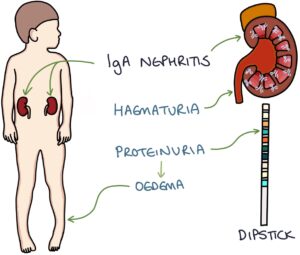
HSP affects the kidneys in around 50% of patients, causing an IgA nephritis. This is sometimes referred to as HSP nephritis. This can lead to microscopic or macroscopic haematuria and proteinuria. If there is more than 2+ of protein on the urine dipstick the child has developed nephrotic syndrome and will have a degree of oedema.
Diagnosis
The most important initial step is to exclude other serious pathology, such as meningococcal septicaemia and leukaemia. Idiopathic thrombocytopenic purpura and haemolytic uraemic syndrome are also differentials for a non-blanching rash.
Investigations to exclude other pathology and assess for organ involvement include:
- Full blood count and blood film for thrombocytopenia, sepsis and leukaemia
- Renal profile for kidney involvement
- Serum albumin for nephrotic syndrome
- CRP for sepsis
- Blood cultures for sepsis
- Urine dipstick for proteinuria
- Urine protein:creatinine ratio to quantify the proteinuria
- Blood pressure for hypertension
There are many different sets of criteria for diagnosing HSP, the most recent being the EULAR/PRINTO/PRES criteria from 2010. This requires the patient to have palpable purpura (not petichiae) + at least one of:
- Diffuse abdominal pain
- Arthritis or arthralgia
- IgA deposits on histology (biopsy)
- Proteinuria or haematuria
Management
Management is supportive, with simple analgesia, rest and proper hydration.
The use of steroids is debatable, with evidence suggesting they may shorten the duration of the illness but not affect long term outcomes or rate of recurrence. Steroids may be considered by specialist doctors in patients with severe gastrointestinal pain or renal involvement.
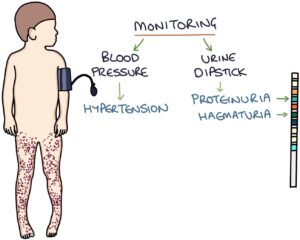
It is important that patients with HSP are monitored closely whilst the illness is active. They need close monitoring with repeated:
- Urine dipstick monitoring for renal involvement
- Blood pressure monitoring for hypertension
Prognosis
Abdominal pain usually settles within a few days. Patients without kidney involvement can expect to fully recover within 4 to 6 weeks. A third of patients have a recurrence of the disease within 6 months. A very small proportion of patients will develop end stage renal failure.
Last updated January 2020
