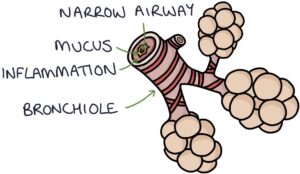
Bronchiolitis describes inflammation and infection in the bronchioles, the small airways of the lungs.
This is usually caused by a virus. Respiratory syncytial virus (RSV) is the most common cause.
Bronchiolitis is very common in winter. Bronchiolitis is generally considered to occur in children under 1 year. It is most common in children under 6 months. It can rarely be diagnosed in children up to 2 years of age, particularly in ex-premature babies with chronic lung disease.
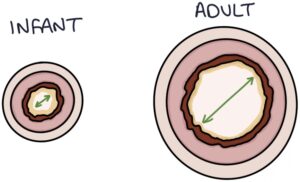
When a virus affects the airways of adults, the swelling and mucus are proportionally so small that it has little noticeable effect on breathing. The airways of infants are very small to begin with, and when there is even the smallest amount of inflammation and mucus in the airway it has a significant effect on the infants ability to circulate air to the alveoli and back out. This causes the harsh breath sounds, wheeze and crackles heard on auscultation when listening to a bronchiolitic baby’s chest.
Presentation
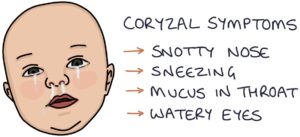
- Coryzal symptoms. These are the typical symptoms of a viral upper respiratory tract infection: running or snotty nose, sneezing, mucus in throat and watery eyes.
- Signs of respiratory distress
- Dyspnoea (heavy laboured breathing)
- Tachypnoea (fast breathing)
- Poor feeding
- Mild fever (under 39ºC)
- Apnoeas are episodes where the child stops breathing
- Wheeze and crackles on auscultation
Signs of Respiratory Distress
One of the foundations of paediatrics is being able to spot the signs of respiratory distress:
- Raised respiratory rate
- Use of accessory muscles of breathing, such as the sternocleidomastoid, abdominal and intercostal muscles
- Intercostal and subcostal recessions
- Nasal flaring
- Head bobbing
- Tracheal tugging
- Cyanosis (due to low oxygen saturation)
- Abnormal airway noises
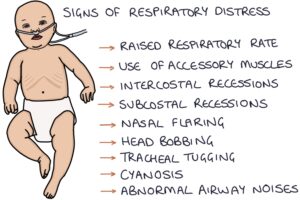
TOM TIP: You should become very confident in listing and spotting the signs of respiratory distress. This is very important when treating children, to distinguish between a well child and an unwell child. Your examiners will expect you to know the signs like the back of your hand.
Abnormal Airway Noises
- Wheezing is a whistling sound caused by narrowed airways, typically heard during expiration
- Grunting is caused by exhaling with the glottis partially closed to increase positive end-expiratory pressure
- Stridor is a high pitched inspiratory noise caused by obstruction of the upper airway, for example in croup
Typical RSV Course
Bronchiolitis usually starts as an upper respiratory tract infection (URTI) with coryzal symptoms. From this point around half get better spontaneously. The other half develop chest symptoms over the first 1-2 days following the onset of coryzal symptoms. Symptoms are generally at their worst on day 3 or 4. Symptoms usually last 7 to 10 days total and most patients fully recover within 2 – 3 weeks. Children who have had bronchiolitis as infants are more likely to have viral induced wheeze during childhood.
Admission
Most infants can be managed at home with advice about when to seek further medical attention. Reasons for admission include:
- Aged under 3 months or any pre-existing condition such as prematurity, Downs syndrome or cystic fibrosis
- 50 – 75% or less of their normal intake of milk
- Clinical dehydration
- Respiratory rate above 70
- Oxygen saturations below 92%
- Moderate to severe respiratory distress, such as deep recessions or head bobbing
- Apnoeas
- Parents not confident in their ability to manage at home or difficulty accessing medical help from home
Management
Typically patients only require supportive management. This involves:
- Ensuring adequate intake. This could be orally, via NG tube or IV fluids depending on the severity. It is important to avoid overfeeding as a full stomach will restrict breathing. Start with small frequent feeds and gradually increase them as tolerated.
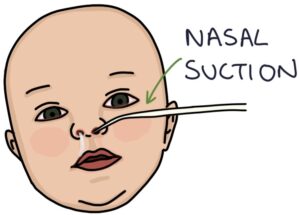
- Saline nasal drops and nasal suctioning can help clear nasal secretions, particularly prior to feeding
- Supplementary oxygen if the oxygen saturations remain below 92%
- Ventilatory support if required
There is little evidence for treatments such as nebulised saline, bronchodilators, steroids and antibiotics.
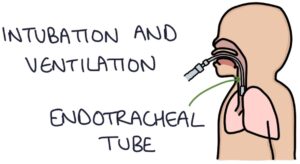
Ventilatory Support
As breathing gets harder, the child gets more tired and less able to adequately ventilate themselves. They may require ventilatory support to maintain their breathing. This is stepped up until they are adequately ventilated:
- High-flow humidified oxygen via tight nasal cannula (i.e. “Airvo” or “Optiflow”). This delivers air and oxygen continuously with some added pressure, helping to oxygenate the lungs and prevent the airways from collapsing. It adds “positive end-expiratory pressure” (PEEP) to maintain the airway at the end of expiration.
- Continuous positive airway pressure (CPAP). This involves using a sealed nasal cannula that performs in a similar way to Airvo or Optiflow, but can deliver much higher and more controlled pressures.
- Intubation and ventilation. This involves inserting an endotracheal tube into the trachea to fully control ventilation.
Assessing Ventilation
Capillary blood gases are useful in severe respiratory distress and in monitoring children who are having ventilatory support.

The most helpful signs of poor ventilation are:
- Rising pCO2, showing that the airways have collapsed and can’t clear waste carbon dioxide.
- Falling pH, showing that CO2 is building up and they are not able to buffer the acidosis this creates. This is a respiratory acidosis. If they are also hypoxic, this is classed as type 2 respiratory failure.
Palivizumab
Palivizumab is a monoclonal antibody that targets the respiratory syncytial virus. A monthly injection is given as prevention against bronchiolitis caused by RSV. It is given to high risk babies, such as ex-premature and those with congenital heart disease.
It is not a true vaccine as it does not stimulate the infant’s immune system. It provides passive protection by circulating the body until the virus is encountered, as which point it works as an antibody against the virus, activating the immune system to fight the virus. The levels of circulating antibodies decrease over time, which is why a monthly injection is required.

Last updated January 2020
