Jaundice describes the condition of abnormally high levels of bilirubin in the blood.
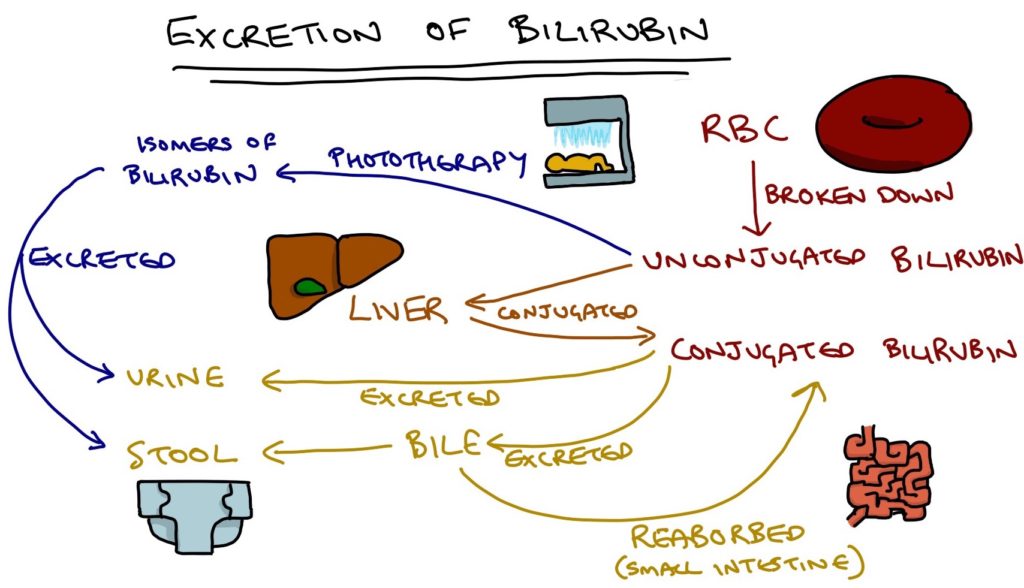
- Red blood cells contain unconjugated bilirubin
- When red blood cells break down, they release unconjugated bilirubin that travels to the liver, becomes conjugated and is then excreted via the biliary system into the stool and via the urine
- Newborn babies and fetuses have a high concentration of red blood cells, that are more fragile than normal red blood cells
- They also have less developed liver function
Physiological Jaundice
- Fetal red blood cells break down and release lots of bilirubin
- Normally this bilirubin is excreted via the placenta, however at birth the foetus no longer has his luxury
- This leads to a normal rise in bilirubin, causing a mild yellowing of skin and sclera from 2-7 days of age and usually resolves completely by 10 days
- The baby remains otherwise healthy and well
Jaundice in Prematurity
- In premature babies, the process of physiological jaundice is exaggerated due to the immature liver
- This increase the risk of complications (kernicterus)
- In premature neonates, total bilirubin levels are monitored
- If total bilirubin reaches a threshold (see local guidelines) treatment is required
- Phototherapy is usually adequate to correct neonatal jaundice
- Extremely high levels require exchange transfusions (rarely)
Phototherapy
- Phototherapy converts unconjugated bilirubin into isomers that can be excreted in the bile and urine without requiring conjugation in the liver
- Involves lying in a cot with minimal clothing and eye patches
- A lightbox shines UV light on baby’s skin
- Exposure is intermitted and bilirubin is closely monitored during treatment
Abnormal Neonatal Jaundice
Jaundice is abnormal when:
- It occurs within 24 hours of birth
- Lasts more than 14 days in full term babies
- Last more than 21 days in premature babies
Caused by increase bilirubin production or decreased clearance
Increased production:
- Haemolytic disease
- Rhesus alloimmunisation
- ABO incompatibility
- Haemorrhage
- Intraventricular haemorrhage
- Cephalohaematoma
- Polycythaemia
- Disseminated intravascular coagulation (secondary to sepsis)
Decreased clearance:
- Prematurity
- Breast milk jaundice
- Neonatal cholestasis
- Extrahepatic biliary atresia
- Increased reabsorption from the liver
- Pyloric stenosis
- Bowel obstruction
- Endocrine disorders
- Hypothyroid
- Hypopituitary
- Gilbert Syndrome
Testing
- Full blood count – for polycythaemia / anaemia
- Measure conjugated bilirubin – elevated levels indicate hepatobiliary cause
- Blood type testing of mother and baby – tests for ABO / Rhesus incompatibility with the mother
- Direct Coombs Test (direct antiglobulin test – for haemolysis
- Check thyroid function – particularly for hypothyroid
Kernicterus
- Now rare due to good treatment of jaundice
- Bilirubin crosses the blood brain barrier
- Excessive bilirubin causes direct damage to the central nervous system
- Presents with less responsive, floppy, drowsy baby with poor feeding
- Leads to permanent damage (cerebral palsy, learning difficulties, deafness)
