Tonsillitis refers to inflammation in the tonsils.
The most common cause of tonsillitis is a viral infection. Viral infections do not require or respond to antibiotics.
The most common cause of bacterial tonsillitis is group A streptococcus (Streptococcus pyogenes). This can be effectively treated with penicillin V (phenoxymethylpenicillin). The most common cause of otitis media, rhinosinusitis and the most common alternative bacterial cause of tonsillitis is Streptococcus pneumoniae.
Other causes:
- Haemophilus influenzae
- Morazella catarrhalis
- Staphylococcus aureus
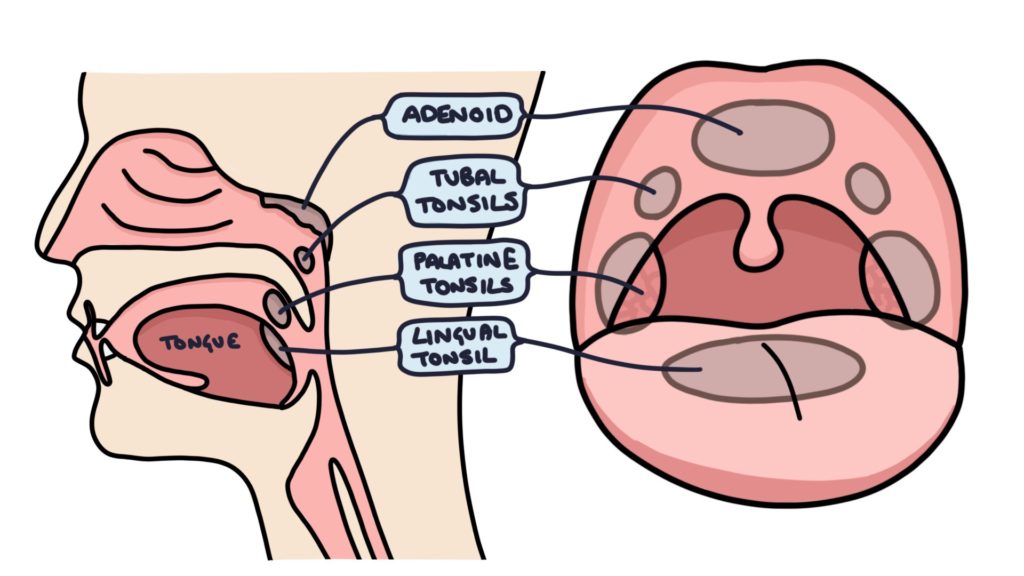
Waldeyer’s Tonsillar Ring
In the pharynx, at the back of the throat, there is a ring of lymphoid tissue. There are six areas of lymphoid tissues, making up the adenoid, tubal tonsils, palatine tonsils and the lingual tonsil. The palatine tonsils are the ones typically infected and enlarged in tonsillitis. These are the tonsils at either side at the back of the throat.
Features of Tonsillitis
A typical presentation is a child with a fever, sore throat and painful swallowing. Children aged 5 to 10 are most often affected, with another peak between ages 15 and 20.
Tonsillitis can present with non-specific symptoms, particularly in younger children. They may present with only a fever, poor oral intake, headache, vomiting or even abdominal pain.
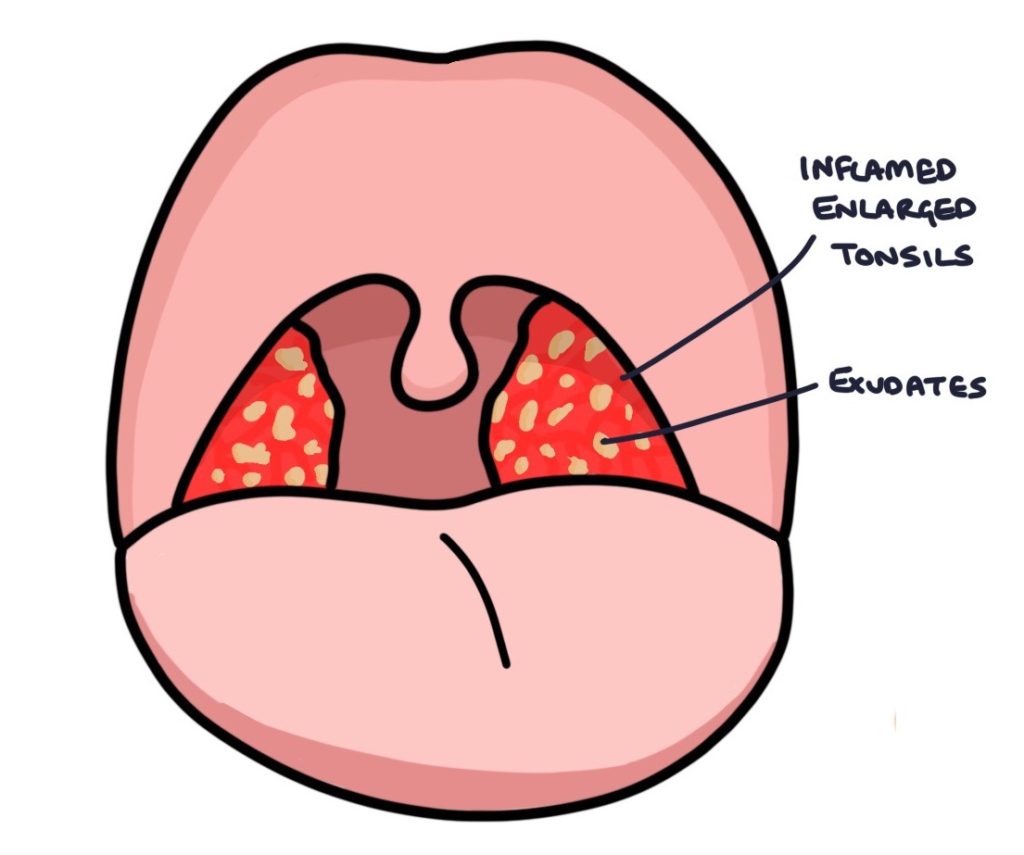
Examination of the throat will reveal red, inflamed and enlarged tonsils, with or without exudates. Exudates are small white patches of pus on the tonsils.
Always examine the ears (otoscopy) to visualising the tympanic membranes and palpate for any cervical lymphadenopathy when assessing a child with suspected tonsillitis.
Centor Criteria
The Centor criteria can be used to estimate the probability that tonsillitis is due to a bacteria infection, and will benefit from antibiotics.
A score of 3 or more gives a 40 – 60 % probability of bacterial tonsillitis, and it is appropriate to offer antibiotics. A point is given if each of the following features are present:
- Fever over 38ºC
- Tonsillar exudates
- Absence of cough
- Tender anterior cervical lymph nodes (lymphadenopathy)
FeverPAIN Score
The FeverPAIN score is an alternative to the Centor criteria. A score of 2 – 3 gives a 34 – 40% probability and 4 – 5 gives a 62 – 65% probability of bacterial tonsillitis:
- Fever during previous 24 hours
- P – Purulence (pus on tonsils)
- A – Attended within 3 days of the onset of symptoms
- I – Inflamed tonsils (severely inflamed)
- N – No cough or coryza
Management
It is important to exclude other serious pathology, such as meningitis, epiglottitis and peritonsillar abscess. When tonsillitis is the most likely diagnosis, calculate the Centor criteria or FeverPAIN score.
Educate patients or parents with likely viral tonsillitis, and give safety net advice about when to seek medical advice. Advise simple analgesia with paracetamol and ibuprofen to control pain and fever. NICE clinical knowledge summaries suggest advising patients to return if the pain has not settled after 3 days or the fever rises above 38.3ºC. If this occurs you can start antibiotics or consider an alternative diagnosis.
Consider prescribing antibiotics if the Centor score is ≥ 3 or the FeverPAIN score is ≥ 4. Also consider antibiotics if they are at risk of more serious infections, for example young infants, immunocompromised patients or those with significant co-morbidity, or there is a history of rheumatic fever.
Delayed prescriptions can be considered. This involves educating patients or parents about the likely viral nature of the sore throat, and providing a prescription that is to be collected only in the event that the symptoms do not improve or worsen in the next 2 – 3 days.
Consider admission if the patient is immunocompromised, systemically unwell, dehydrated, has stridor, respiratory distress or evidence of a peritonsillar abscess or cellulitis.
Choice of Antibiotic
Penicillin V (also called phenoxymethylpenicillin) for a 10 day course is typically first line. The trouble with penicillin V is it tastes bad, so young children requiring syrups are often reluctant to take it. Amoxicillin has a better taste but is not part of the guidelines.
Clarithromycin is the first line choice in true penicillin allergy.
Complications
- Chronic tonsillitis
- Peritonsillar abscess, also known as quinsy
- Otitis media if the infection spreads to the inner ear
- Scarlet fever
- Rheumatic fever
- Post-streptococcal glomerulonephritis
- Post-streptococcal reactive arthritis
Last updated January 2020
