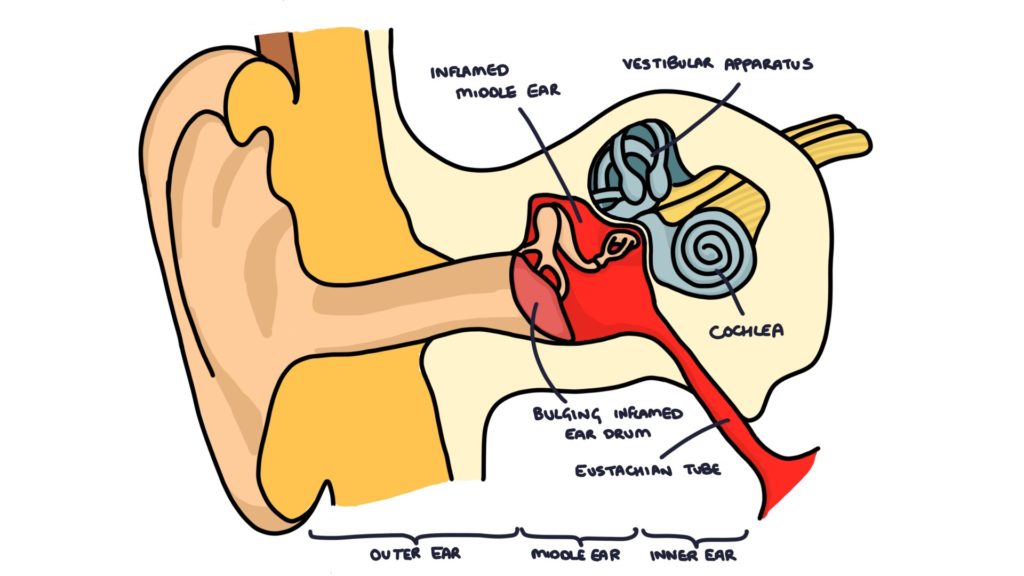
Otitis media is the name given to an infection in the middle ear. The middle ear is the space that sits between the tympanic membrane (ear drum) and the inner ear. This is where the cochlea, vestibular apparatus and nerves are found. It is a very common site of infection in children. The bacteria enter from the back of the throat through the eustachian tube. A bacterial infection of the middle ear is often preceded by a viral upper respiratory tract infection.
Bacteria
The most common bacterial causes of otitis media, as well as other ENT infections such as rhino-sinusitis and tonsillitis is streptococcus pneumoniae.
Other common causes include:
- Haemophilus influenzae
- Moraxella catarrhalis
- Staphylococcus aureus
Presentation
Otitis media typically presents with ear pain, reduced hearing in the affected ear and general symptoms of upper airway infection such as fever, cough, coryzal symptoms, sore throat and feeling generally unwell.
When the infection affects the vestibular system it can cause balance issues and vertigo. When the tympanic membrane has perforated there may be discharge from the ear.
It is worth noting that symptoms can be very non-specific, particularly in young children and infants. They may present with symptoms of fever, vomiting, irritability, lethargy or poor feeding. It is always worth examining the ears in unwell children.
Examination
Always examine both ears and the throat of unwell children. These are common sites of infection and can produce non-specific symptoms. Use an otoscope to visualise the tympanic membrane whilst gently pulling the pinna up and backwards. It may be difficult to visualise the tympanic membrane if there is significant discharge or wax in the ear canal.
In a normal child the tympanic membrane should be “pearly-grey”, translucent and slightly shiny. You should be able to visualise the malleus through the membrane and a cone of light reflecting the light of the otoscope.
Otitis media will give a bulging, red, inflamed looking membrane. When there is a perforation, you may see discharge in the ear canal and a hole in the tympanic membrane.
Management
Consider referral to paediatrics for assessment or admission if symptoms are severe or there is diagnostic doubt. Always refer for specialist assessment and to consider admission in infants younger than 3 months with a temperature above 38ºC or 3 – 6 months with a temperature higher than 39ºC.
Most cases of otitis media will resolve without antibiotics, and NICE guidelines from 2018 highlight the importance of not providing antibiotics for otitis media. They state that most cases of otitis media will resolve within 3 days without antibiotics, but it can last for up to a week. Complications (mainly mastoiditis) are rare. Give simple analgesia to help with pain and fever.
There are three options regarding prescribing antibiotics to patients with otitis media:
- Immediate antibiotics
- Delayed prescription
- No antibiotics
Consider prescribing antibiotics at the initial presentation in patients who have significant co-morbidities, are systemically unwell or are immunocompromised. Children less than 2 years with bilateral otitis media and children with otorrhoea (discharge) are more likely to benefit from antibiotics.
Consider a delayed prescription that can be collected and used after 3 days if symptoms have not improved or have worsened at any time. This can be useful with patients that are very keen on antibiotics or where you suspect they might get worse.
The first line choice of antibiotic is amoxicillin for 5 days. Alternatives are erythromycin and clarithromycin.
Always safety-net, offering education and advice to patients and parents on when to seek further medical attention.
Complications
- Otitis medial with effusion
- Hearing loss (usually temporary)
- Perforated eardrum
- Recurrent infection
- Mastoiditis (rare)
- Abscess (rare)
Last updated January 2020
