Adrenal insufficiency is where the adrenal glands do not produce enough steroid hormones, particularly cortisol and aldosterone. Steroids are essential for life. Therefore, the condition is life threatening unless the hormones are replaced.
Addison’s disease refers a the specific condition where the adrenal glands have been damaged, resulting in reduced secretion of cortisol and aldosterone. This is also called primary adrenal insufficiency. The most common cause is autoimmune.
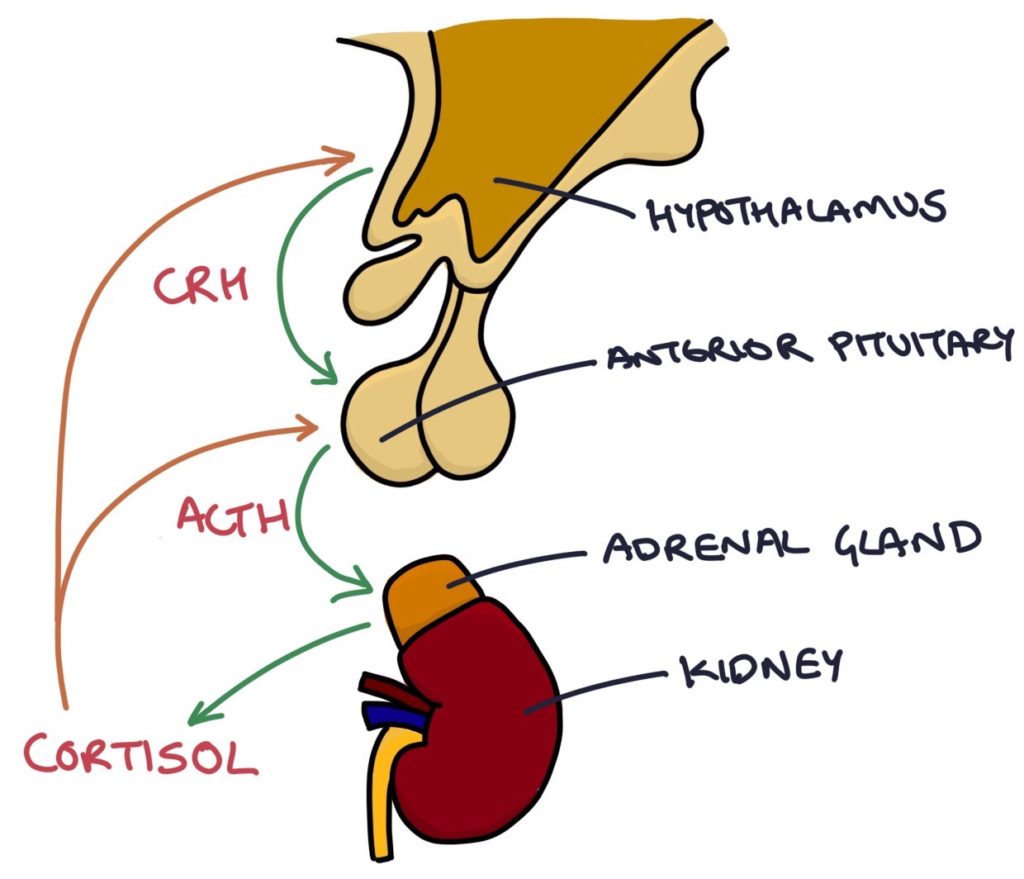
Secondary adrenal insufficiency is a caused by inadequate ACTH stimulating the adrenal glands, resulting in low levels of cortisol being released. This is the result of loss or damage to the pituitary gland. This can be due to congenital underdevelopment (hypoplasia) of the pituitary gland, surgery, infection, loss of blood flow or radiotherapy.
Tertiary adrenal insufficiency is the result of inadequate CRH release by the hypothalamus. This is usually the result of patients being on long term oral steroids (for more than 3 weeks) causing suppression of the hypothalamus. When the exogenous steroids are suddenly withdrawn the hypothalamus does not “wake up” fast enough and endogenous steroids are not adequately produced. Therefore, long term steroids should be tapered slowly to allow time for the adrenal axis to regain normal function.
Features in Babies
- Lethargy
- Vomiting
- Poor feeding
- Hypoglycaemia
- Jaundice
- Failure to thrive
Features in Older Children
- Nausea and vomiting
- Poor weight gain or weight loss
- Reduced appetite (anorexia)
- Abdominal pain
- Muscle weakness or cramps
- Developmental delay or poor academic performance
- Bronze hyperpigmentation to skin in Addison’s caused by high ACTH levels. ACTH stimulates melanocytes.
Investigations
All children with suspected adrenal insufficiency should have U&Es (hyponatraemia and hyperkalaemia) and blood glucose (hypoglycaemia) levels checked.
Test for the diagnosis with cortisol, ACTH, aldosterone and renin levels, prior to administering steroids if possible.
Addisons Disease (Primary Adrenal Failure)
- Low cortisol
- High ACTH
- Low aldosterone
- High renin
Secondary Adrenal Insufficiency
- Low cortisol
- Low ACTH
- Normal aldosterone
- Normal renin
Short Synacthen Test (ACTH Stimulation Test)
The short synacthen test can be used to confirm adrenal insufficiency. It is ideally performed in the morning when the adrenal glands are the most “fresh”. The test involves giving synacthen, which is synthetic ACTH. The blood cortisol is measured at baseline, 30 and 60 minutes after administration. The synthetic ACTH will stimulate healthy adrenal glands to produce cortisol. The cortisol level should at least double in response to synacthen. A failure of cortisol to rise (less than double the baseline) indicates primary adrenal insufficiency (Addison’s disease).
Management
Treatment of adrenal insufficiency is with replacement steroids titrated to signs, symptoms and electrolytes. Hydrocortisone is a glucocorticoid hormone used to replace cortisol. Fludrocortisone is a mineralocorticoid hormone used to replace aldosterone if aldosterone is also insufficient.
Patients are given a steroid card and an emergency ID tag to inform emergency services they are dependent on steroids for life. Steroids are essential to life, therefore should not be missed. Doses are increased during an acute illness to match the normal steroid response to illness.
Patients should be followed up by a specialist paediatric endocrinologist and have an individual care plan. They are monitored closely for:
- Growth and development
- Blood pressure
- U&Es
- Glucose
- Bone profile
- Vitamin D
During Acute Illness (Sick Day Rules)
Usually minor coughs or colds without fever not not require a change in medications. If they are more unwell, for example with a temperature over 38ºC or vomiting and diarrhoea, there is an increased demand on the body for steroids to deal with the illness. There is also an increased risk of hypoglycaemia. They need to have an individual care plan documenting exactly how to manage acute illnesses:
- The dose of steroid needs to be increased and given more regularly until the illness has completely resolved.
- Blood sugar needs to be monitored closely and they need to eat foods containing carbohydrates regularly.
- With diarrhoea or vomiting, they need an IM injection of steroid at home and likely required admission for IV steroids.
Addisonian Crisis (AKA Adrenal Crisis)
Addisonian crisis is the term used to describe an acute presentation of severe Addisons, where the absence of steroid hormones result in a life threatening presentation. Patients can be very unwell. They present with:
- Reduced consciousness
- Hypotension
- Hypoglycaemia, hyponatraemia and hyperkalaemia
Adrenal crisis can be the first presentation of Addison’s disease or triggered by infection, trauma or other acute illness in someone with established Addison’s. It can also occur in patients on long term steroids that have suppressed their natural steroid production, if that patient stops taking the steroids abruptly.
Do not wait to perform investigations and establish a definitive diagnosis before initiating treatment for someone with suspected Addisonian crisis, as the condition is life threatening and immediate treatment is required.
Management of Addisonian Crisis
- Intensive monitoring if they are acutely unwell
- Parenteral steroids (i.e. IV hydrocortisone)
- IV fluid resuscitation
- Correct hypoglycaemia
- Careful monitoring of electrolytes and fluid balance
Last updated August 2019
