Adrenal insufficiency is where the adrenal glands do not produce enough steroid hormones, particularly cortisol and aldosterone. Steroids are essential for life, making the condition life-threatening.
Glucocorticoids and Mineralocorticoids
The adrenal glands produce two types of steroid hormones:
- Glucocorticoid (cortisol)
- Mineralocorticoid (aldosterone)
Glucocorticoids (e.g., cortisol) help the body cope with stress. Cortisol has several actions within the body:
- Increases alertness
- Inhibits the immune system and reduces inflammation
- Inhibits bone formation
- Raises blood glucose
- Increases metabolism
- Supports cardiovascular function (heart rate, blood pressure and cardiac output)
Mineralocorticoids (e.g., aldosterone) help regulate the balance of electrolytes and blood pressure. They act on the nephrons in the kidneys to:
- Increase sodium reabsorption from the distal tubule
- Increase potassium secretion from the distal tubule
- Increase hydrogen secretion from the collecting ducts
The Adrenal Axis
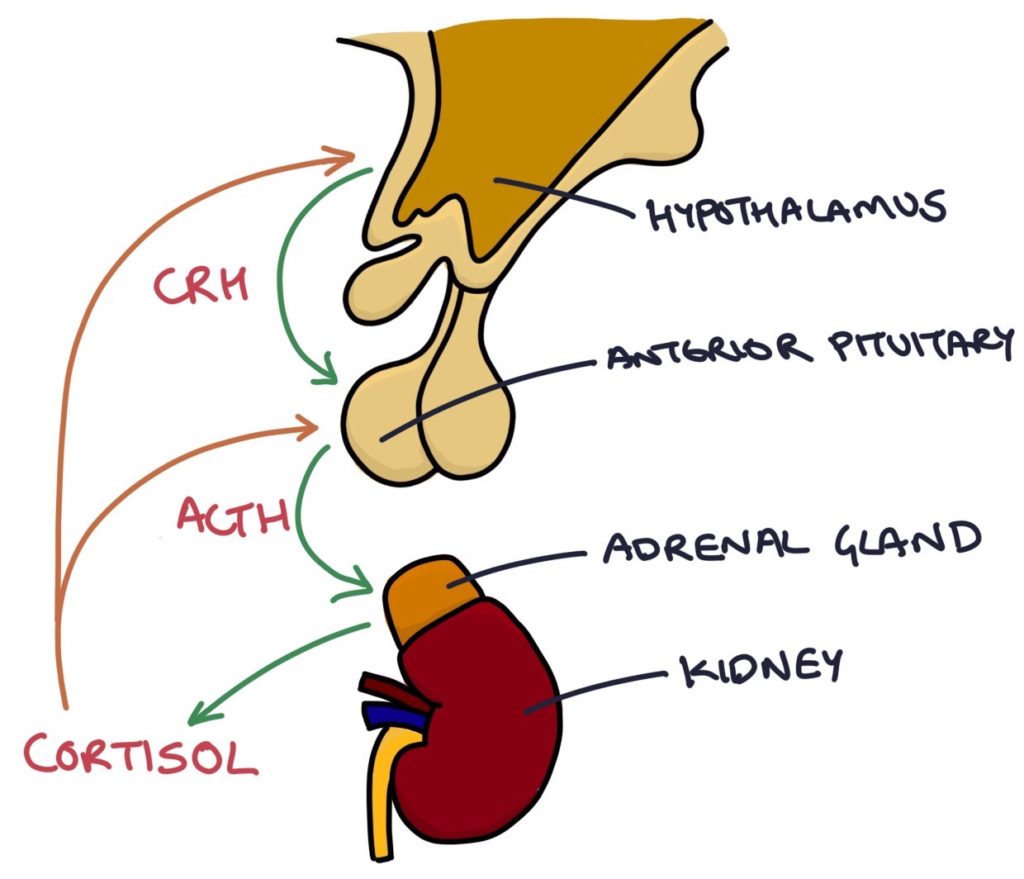
The hypothalamus releases corticotropin-releasing hormone (CRH), which stimulates the anterior pituitary to release adrenocorticotropic hormone (ACTH). ACTH stimulates the adrenals to release cortisol.
The adrenal axis is controlled by negative feedback. Raised cortisol suppresses the release of CRH and ACTH by the hypothalamus and anterior pituitary.
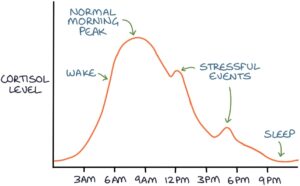
Cortisol is released in pulses throughout the day and in response to a stressful stimulus (it is a “stress hormone”). It has diurnal variation, meaning it is high and low at different times of the day. Typically, cortisol peaks in the early morning, triggering us to wake up and get going, and is at its lowest late in the evening, prompting us to relax and fall asleep.
Causes
Addison’s disease refers specifically to when the adrenal glands have been damaged, resulting in reduced cortisol and aldosterone secretion. This is called primary adrenal insufficiency. It is primary, as the problem is with the direct source of cortisol (the adrenal glands). In infants, the most common cause is congenital adrenal hyperplasia. It can also be autoimmune, where the immune system attacks and damages the adrenal glands.
Congenital adrenal hyperplasia is an autosomal recessive genetic condition causing a deficiency of the 21-hydroxylase enzyme, which converts progesterone to aldosterone and cortisol. Deficiency of this enzyme causes the underproduction of cortisol and aldosterone and overproduction of androgens from birth.
Secondary adrenal insufficiency occurs when inadequate ACTH is produced by the pituitary gland (e.g., congenital hypopituitarism or acquired damage). Suppression by exogenous steroids (e.g., long-term treatment with prednisolone) may be described as secondary or tertiary adrenal insufficiency. Inadequate ACTH means low adrenal stimulation and insufficient cortisol release. It is secondary, as the problem is one step back from the adrenal glands.
Tertiary adrenal insufficiency occurs when the hypothalamus produces inadequate CRH, usually due to suppression by exogenous steroids (e.g., long-term prednisolone). Inadequate CRH and ACTH mean low adrenal stimulation and reduced cortisol secretion. It is tertiary, as the problem is two steps back from the adrenal glands.
Presentation
Presenting features in infants include:
- Failure to gain weight
- Poor feeding
- Lethargy
- Vomiting
- Hypoglycaemia
- Jaundice
Presenting features in older children include:
- Poor weight gain or weight loss
- Lethargy
- Reduced appetite (anorexia)
- Abdominal pain
- Craving salt
- Dehydration
- Vomiting
- Muscle weakness or cramps
- Skin hyperpigmentation in Addison’s caused by high ACTH levels (ACTH stimulates melanocytes)
Biochemistry Results
Low cortisol leads to hypoglycaemia (low glucose).
Low aldosterone leads to:
- Hyponatraemia (low sodium)
- Hyperkalaemia (raised potassium)
ACTH results depend on the cause:
- Raised ACTH occurs with primary adrenal insufficiency, due to a lack of negative feedback
- Low ACTH occurs in secondary and tertiary adrenal insufficiency
Short Synacthen Test (ACTH Stimulation Test)
The short Synacthen test (or ACTH stimulation test) is used to diagnose primary adrenal insufficiency. It involves giving a dose of Synacthen (synthetic ACTH) and monitoring the blood cortisol before and at 30 and 60 minutes after the dose.
Synthetic ACTH stimulates healthy adrenal glands to produce cortisol. A failure of the cortisol levels to at least double indicates primary adrenal insufficiency. The damaged and dysfunctional adrenal glands fail to respond to the ACTH.
Management
A specialist paediatric endocrinologist will provide an individual care plan and follow-up. Children are monitored closely for their growth and development.
Treatment of adrenal insufficiency is with replacement steroids, titrated to signs, symptoms and electrolytes:
- Hydrocortisone (a glucocorticoid) is used to replace cortisol
- Fludrocortisone (a mineralocorticoid) is used to replace aldosterone, if aldosterone is also insufficient
Patients are given a steroid card, ID tag and emergency letter to alert emergency services that they depend on steroids for life. Doses should not be missed, as they are essential to life.
Sick day doses (higher than normal doses of hydrocortisone) are given during an acute illness to match the normal steroid response to illness.
Patients and close contacts are taught to give intramuscular hydrocortisone in an emergency.
Adrenal Crisis
Adrenal crisis, also known as Addisonian crisis, describes an acute presentation of severe adrenal insufficiency, where the absence of steroid hormones leads to a life-threatening emergency. It presents with:
- Reduced consciousness
- Hypotension (low blood pressure)
- Hypoglycaemia (low blood glucose)
- Hyponatraemia (low sodium) and hyperkalaemia (high potassium)
It may be the initial presentation of adrenal insufficiency or may have been triggered by infection, trauma or other acute illness in established adrenal insufficiency.
Management involves:
- ABCDE approach to initial assessment and arrange transfer to hospital
- Intramuscular or intravenous hydrocortisone
- Intravenous fluids
- Correct hypoglycaemia (e.g., IV dextrose)
- Careful monitoring of electrolytes and fluid balance
Last updated February 2025
Now, head over to members.zerotofinals.com and test your knowledge of this content. Testing yourself helps identify what you missed and strengthens your understanding and retention.