A ventricular septal defect (VSD) is a congenital hole in the septum (wall) between the left and right ventricles. The hole may be small, with minimal effects, or larger, even affecting the entire septum. They may be associated with Down’s syndrome or Turner’s syndrome.
Pathophysiology
The pressure is higher in the left ventricle compared with the right. Therefore, blood flows from the left ventricle to the right ventricle. Blood continues to flow to the lungs to get oxygenated so the patient does not become cyanotic. However, the left-to-right shunt can cause right-sided overload, right heart failure and pulmonary hypertension.
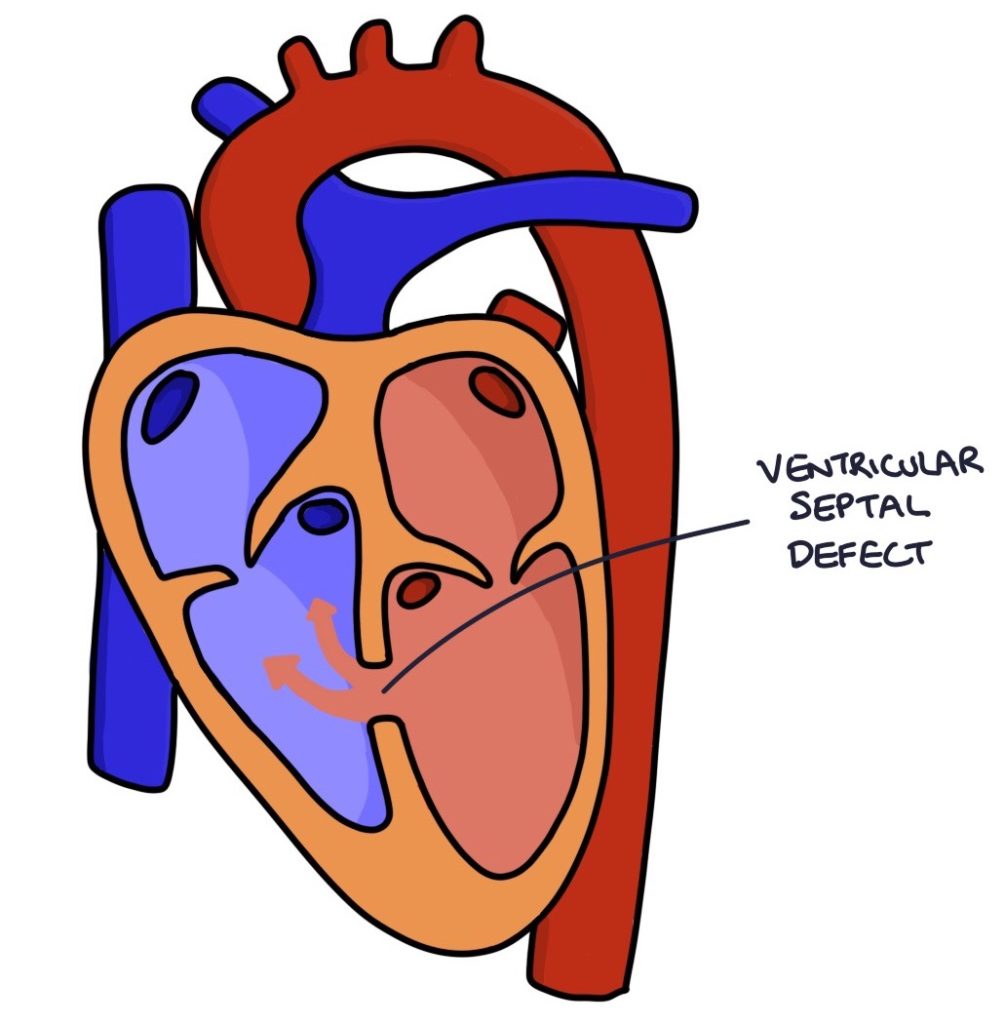
When the pulmonary pressure exceeds the systemic pressure, blood starts to flow from the right ventricle to the left ventricle, becoming a right-to-left shunt. Blood bypasses the lungs, and the patient becomes cyanotic. The change to a right-to-left shunt with the development of cyanosis is called Eisenmenger syndrome.
Presentation
Often, VSDs are initially symptomless, and patients can present as late as adulthood. They may detected during antenatal scans or the newborn baby check.
Typical symptoms include:
- Poor feeding
- Dyspnoea
- Tachypnoea
- Failure to thrive
Examination Findings
VSDs cause a pan-systolic murmur heard loudest at the left lower sternal border in the third and fourth intercostal spaces. There may be a systolic thrill on palpation.
TOM TIP: Causes of a pan-systolic murmur: VSDs, mitral regurgitation and tricuspid regurgitation.
Management
An echocardiogram confirms the diagnosis.
A paediatric cardiologist will manage patients with a VSD. Management options include:
- Active monitoring (small defects may close on their own)
- Percutaneous transvenous catheter closure (via the femoral vein)
- Open-heart surgery
VSDs increase the risk of infective endocarditis.
Last updated January 2025
Now, head over to members.zerotofinals.com and test your knowledge of this content. Testing yourself helps identify what you missed and strengthens your understanding and retention.

