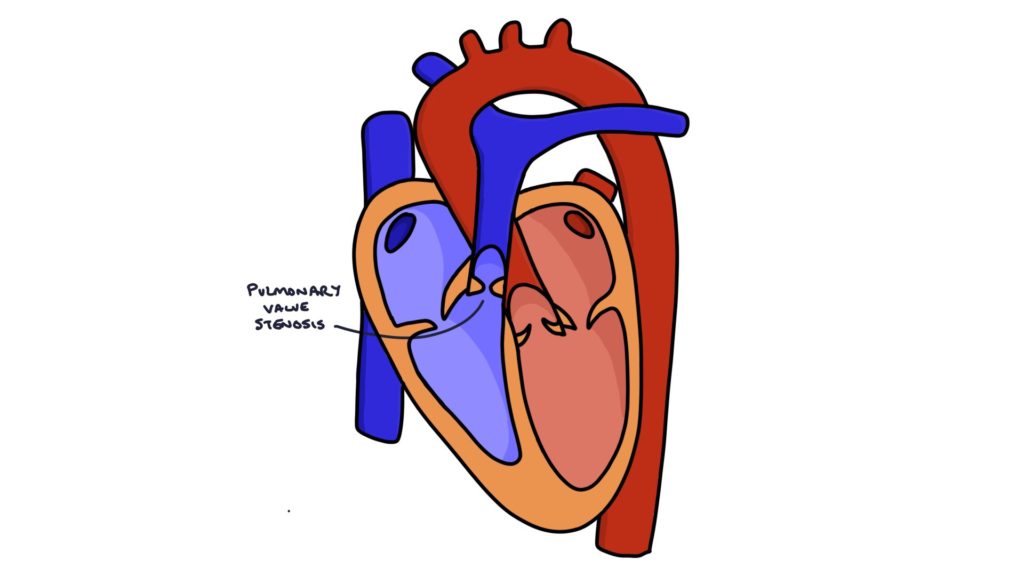
The pulmonary valve lets blood flow from the right ventricle to the pulmonary arteries and prevents blood from flowing back into the right ventricle. It usually consists of three leaflets. When these leaflets develop abnormally, becoming thickened or fused, it can result in a narrow opening. This is called congenital pulmonary valve stenosis.
Congenital pulmonary valve stenosis may be associated with:
- Tetralogy of Fallot
- William syndrome
- Noonan syndrome
- Congenital rubella syndrome
Presentation
Pulmonary stenosis is often asymptomatic.
More significant pulmonary valve stenosis can present with:
- Fatigue on exertion
- Shortness of breath
- Dizziness
- Syncope (fainting)
Signs on examination may include:
- Ejection systolic murmur heard loudest at the pulmonary area (second intercostal space, left sternal border)
- Palpable thrill in the pulmonary area
- Right ventricular heave (due to right ventricular hypertrophy)
- Raised JVP with giant a waves
- Widely split second heart sound
The narrow pulmonary valve prolongs the time it takes for the right ventricle to empty. By contrast, the left ventricle empties relatively quickly through a healthy aortic valve. Closure of the pulmonary valve is delayed and occurs noticeably later than the closure of the aortic valve. This causes a widely split second heart sound, meaning that two separate sounds are heard, rather than the usual single second heart sound.
Management
An echocardiogram confirms the diagnosis.
Mild, asymptomatic disease may not require any intervention.
Treatment options include:
- Percutaneous balloon pulmonary valvuloplasty (inflating a balloon to stretch the valve via a catheter)
- Surgical aortic valvotomy
- Valve replacement
Last updated January 2025
Now, head over to members.zerotofinals.com and test your knowledge of this content. Testing yourself helps identify what you missed and strengthens your understanding and retention.

