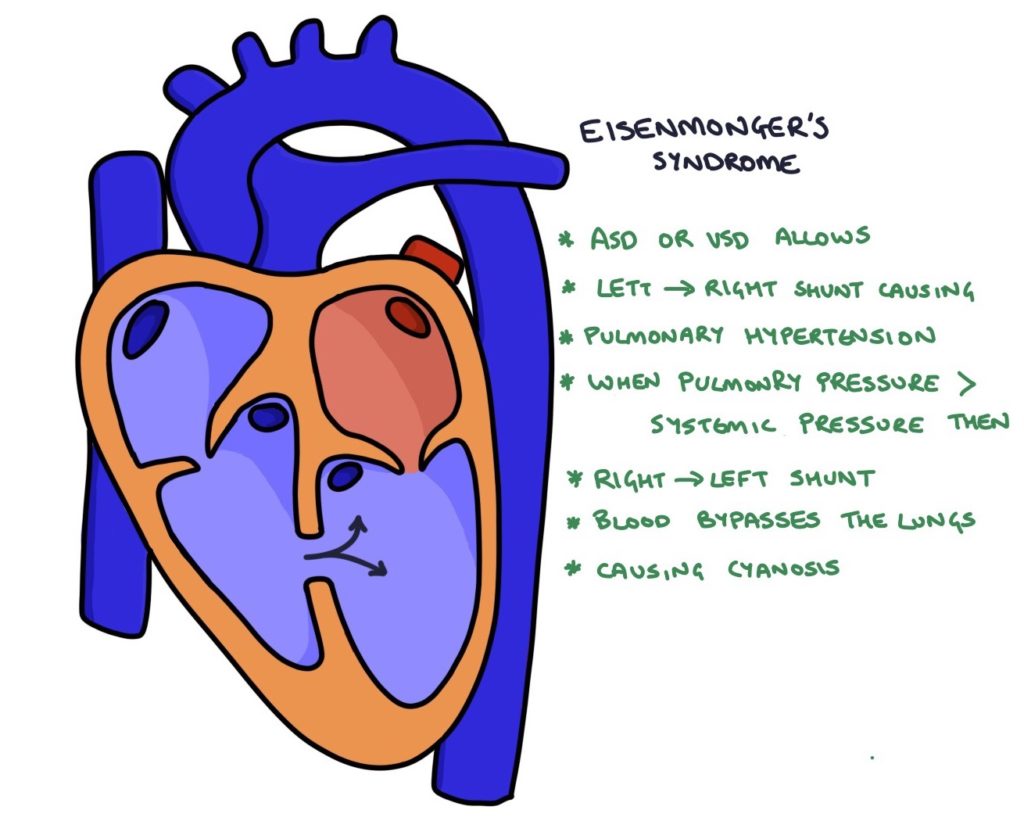
Eisenmenger syndrome occurs when blood flows from the right to the left side of the heart across a structural heart lesion, bypassing the lungs. Three underlying lesions can result in Eisenmenger syndrome:
- Atrial septal defect
- Ventricular septal defect
- Patent ductus arteriosus
Eisenmenger syndrome can develop within a few years with large lesions or in adulthood with small shunts. It can develop more rapidly during pregnancy.
Pathophysiology
The systemic pressure (left side) is greater than the pulmonary pressure (right side). This means that blood will flow from the left side to the right side across a defect, described as a left-to-right shunt. Blood still travels to the lungs and gets oxygenated, so the patient does not become cyanotic.
Over time, the extra blood flowing into the right side of the heart and the lungs increases the pressure in the pulmonary vessels, causing pulmonary hypertension. When the pulmonary pressure exceeds the systemic pressure, blood begins to flow from the right to the left side of the heart across the defect, described as a right-to-left shunt. Deoxygenated blood bypasses the lungs and enters the body, causing cyanosis.
Cyanosis refers to the blue discolouration of skin caused by a lack of oxygen. The bone marrow responds to low oxygen saturation by producing more red blood cells and haemoglobin to increase the oxygen-carrying capacity of the blood. This results in polycythaemia, which is a high concentration of haemoglobin in the blood. Polycythaemia gives patients a plethoric complexion (reddish skin) and increases the plasma viscosity and risk of thrombus formation.
Examination Findings
Signs of pulmonary hypertension:
- Right ventricular heave (the right ventricle contracts forcefully against increased pressure in the lungs)
- Loud P2 (forceful shutting of the pulmonary valve)
- Raised JVP
- Peripheral oedema
Murmurs related to the underlying septal defect:
- Atrial septal defect: Mid-systolic, crescendo-decrescendo murmur loudest at the upper left sternal border
- Ventricular septal defect: Pan-systolic murmur loudest at the left lower sternal border
- Patent ductus arteriosus: Continuous crescendo-decrescendo “machinery” murmur
Findings related to the right-to-left shunt and chronic hypoxia:
- Cyanosis
- Finger clubbing
- Dyspnoea (shortness of breath)
- Plethoric complexion (reddish skin related to polycythaemia)
Management
Early management of the underlying lesion can prevent Eisenmenger syndrome.
A heart-lung transplant is the only definitive treatment once Eisenmenger syndrome develops.
Management of complications may involve:
- Oxygen for shortness of breath
- Sildenafil and bosentan for pulmonary hypertension
- Diuretics for oedema
- Anti-arrhythmic drugs for arrhythmia
- Venesection for polycythaemia
- Anticoagulation for thrombosis
- Antibiotics for infective endocarditis
Prognosis
Eisenmenger syndrome reduces life expectancy by around 20 years compared with healthy individuals. The main causes of death are heart failure, infection, thromboembolism and haemorrhage. The mortality can be up to 50% in pregnancy.
Last updated January 2025
Now, head over to members.zerotofinals.com and test your knowledge of this content. Testing yourself helps identify what you missed and strengthens your understanding and retention.

