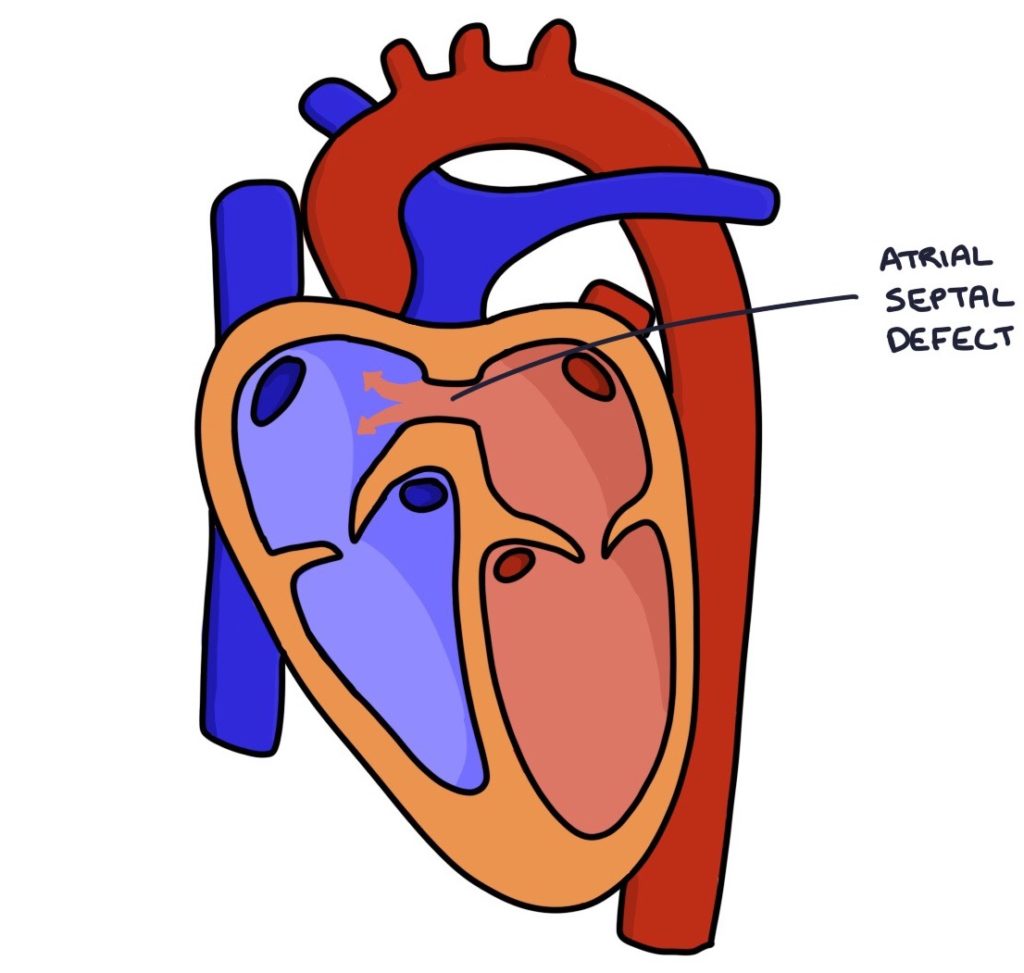
An atrial septal defect is a defect (a hole) in the septum (the wall) between the two atria. This connects the right and left atria, allowing blood to flow between them.
Pathophysiology
During the development of the fetus, the left and right atria are connected. Two walls called the septum primum and septum secundum grow across the gap between the atria. They eventually fuse with the endocardial cushion to separate the two atria. There is a small hole in the septum secundum called the foramen ovale. The foramen ovale usually closes at birth. Defects in the septum primum or septum secundum lead to an atrial septal defect.
An atrial septal defect leads to a shunt, with blood moving between the two atria. Initially, higher pressure in the left atrium means that blood moves from the left atrium to the right atrium. There is a left-to-right shunt. Blood continues to flow to the pulmonary vessels and lungs to get oxygenated, and the patient does not become cyanotic. However, increased flow to the right side of the heart leads to right-sided overload, increased pulmonary pressure and right heart strain. Eventually, this can cause pulmonary hypertension and right heart failure.
When the pulmonary pressure exceeds the systemic pressure, blood starts to flow from the right atrium to the left atrium, becoming a right-to-left shunt. Blood bypasses the lungs, and the patient becomes cyanotic. The change to a right-to-left shunt with the development of cyanosis is called Eisenmenger syndrome.
Types
The types of atrial septal defect, from most to least common, are:
- Patent foramen ovale, where the foramen ovale fails to close (not strictly classified as an ASD)
- Ostium secundum, where the septum secundum fails to fully close
- Ostium primum, where the septum primum fails to fully close (tends to lead to an atrioventricular septal defect)
Complications
- Stroke in the context of venous thromboembolism (see below)
- Atrial fibrillation or atrial flutter
- Pulmonary hypertension and right-sided heart failure
- Eisenmenger syndrome
TOM TIP: Normally when patients have a deep vein thrombosis (DVT) that breaks away and becomes an embolus, the clot travels through the right side of the heart to the lungs and becomes a pulmonary embolism. With an ASD, the clot is able to travel across the ASD, through the left side of the heart and into the systemic circulation. It can then travel up to the brain, causing a large stroke. An exam question may feature a patient with a DVT who develops a stroke and you have to identify that they have had a lifelong asymptomatic ASD.
Presentation
Atrial septal defects cause a mid-systolic, crescendo-decrescendo murmur loudest at the upper left sternal border. There is a fixed split second heart sound.
Splitting of the second heart sound is where you hear the closure of the aortic and pulmonary valves at slightly different times. This can be normal with inspiration. A “fixed split” second heart sound means the split does not change with inspiration or expiration. In an atrial septal defect, blood flows from the left to the right atrium across the atrial septal defect, increasing the volume of blood the right ventricle has to empty before the pulmonary valve can close. The pulmonary valve closes later than the aortic valve, causing a split second heart sound that does not vary with respiration.
Atrial septal defects may be detected on antenatal scans or newborn examinations. It may be asymptomatic in childhood and present in adulthood with dyspnoea, heart failure or stroke. Typical symptoms in childhood are:
- Shortness of breath
- Difficulty feeding
- Poor weight gain
- Lower respiratory tract infections
There appears to be a link between migraine with aura and patent foramen ovale. However, there are no recommendations in the guidelines for testing or treating patients with migraines for a PFO. It is unclear whether testing or treating improves symptoms or outcomes.
Management
An echocardiogram confirms the diagnosis.
A paediatric cardiologist will manage patients with an ASD.
Management options include:
- Active monitoring (small defects may close on their own)
- Percutaneous transvenous catheter closure (via the femoral vein)
- Open-heart surgery
Last updated November 2024
Now, head over to members.zerotofinals.com and test your knowledge of this content. Testing yourself helps identify what you missed and strengthens your understanding and retention.

