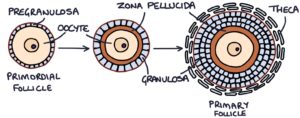
Primordial follicles each contain a primary oocyte. The oocytes are the germ cells (first generation of sex cell) that eventually undergo meiosis to become the mature ovum, ready for fertilisation. They contain the full 46 chromosomes. These primordial follicles and oocytes spend the majority of their lives in a resting state inside the ovaries, waiting for their time to develop. The primary oocyte is contained within the pregranulosa cells, surrounded by the outer basal lamina layer.
Development of the Primary Follicle
Primordial follicles grow and become primary follicles. These primary follicles have three layers:
- The primary oocyte in the centre
- The zona pellucida
- The cuboidal shaped granulosa cells
The granulosa cells secrete the material that becomes the zona pellucida. They also secrete oestrogen.
As the follicles grow larger, they develop a further surrounding layer called the theca folliculi. The inner layer of the theca folliculi is called the theca interna. The theca interna secretes androgen hormones. The outer layer, called the theca externa, is made up of connective tissue cells containing smooth muscle and collagen.
Development of the Secondary Follicle
The process of primordial follicles maturing into primary and secondary follicles is always occurring, independent of the menstrual cycle. As primary follicles become secondary follicles, they grow larger and develop small fluid-filled gaps between the granulosa cells. Once the follicles reach the secondary follicle stage, they have receptors for follicle stimulating hormone (FSH). Further development after the secondary follicle stage requires stimulation from FSH. At the start of the menstrual cycle, FSH stimulates further development of the secondary follicles.
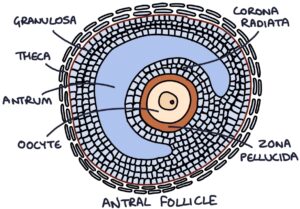
Development of the Antral Follicles
With further development, the secondary follicle develops a single large fluid-filled area within the granulosa cells called the antrum. Antrum refers to a natural chamber within a structure. This is the antral follicle stage. This antrum fills with increasing amounts of fluid, making the follicle expand rapidly. The corona radiata is made of granulosa cells, and surrounds the zona pellucida and the oocyte.
At this point, one of the follicles becomes the dominant follicle. The other follicles start to degrade, while the dominant follicle grows to become a mature follicle. This follicle bulges through the wall of the ovary.
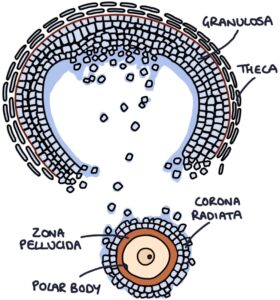
Ovulation
When there is a surge of luteinising hormone (LH) from the pituitary, it causes the smooth muscle of the theca externa to squeeze, and the follicle to burst. Follicular cells also release digestive enzymes that puncture a hole in the wall of the ovary, allowing the ovum to pass escape. The oocyte is released into the area surrounding the ovary. At this point, it is floating in the peritoneal cavity, but it is quickly swept up by the fimbriae of the fallopian tubes.
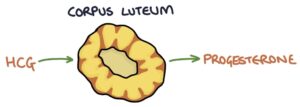
Corpus Luteum
The leftover parts of the follicle collapse and turn a yellow colour. The collapsed follicle becomes the corpus luteum. The cells of the granulosa and theca interna become luteal cells. Luteal cells secrete steroid hormones, most notably progesterone. The corpus luteum persists in response to human chorionic gonadotropin (HCG) from a fertilised blastocyst when pregnancy occurs. When fertilisation does not occur, the corpus luteum degenerates after 10 to 14 days.
Fertilisation
Just before and around the time of ovulation, the primary oocyte undergoes meiosis. This process splits the full 46 chromosomes in the oocyte (a diploid cell) into two, leaving only 23 chromosomes (a haploid cell). The other 23 chromosomes float off to the side and become something called a polar body. It is then a secondary oocyte.
The female egg (ovum) at this stage still has the surrounding layers from its time in the follicle. In the middle is the oocyte with the first polar body, surrounded by the zona pellucida and the granulosa cells that make up the corona radiata.
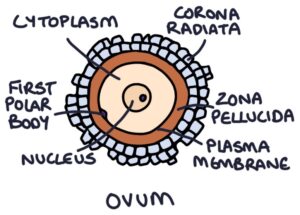
When sperm from the male enter the fallopian tube via the vagina and uterus, they will attempt to penetrate the corona radiata and zona pellucida to fertilise the egg. Usually, only one sperm will get through before the surrounding layers shut the other sperm out.
When a sperm enters the egg, the 23 chromosomes of the egg multiply into two sets. One set of 23 chromosomes combine with the 23 chromosomes from the sperm to form a diploid set of 46 chromosomes, and the other set of 23 chromosomes float off to the side and create the second polar body.
Development of the Blastocyst
The combination of the 23 chromosomes from the egg and 23 chromosomes from the sperm combine to form a fertilised cell called a zygote. This cell divides rapidly to create a mass of cells called the morula. During this process, the mass of cells travels along the fallopian tube toward the uterus.
While travelling, a fluid-filled cavity gathers within the group of cells, and it becomes a blastocyst. The blastocyst contains the main group of cells in the middle, called the embryoblast. Alongside the embryoblast is a fluid-filled cavity called the blastocele. Surrounding the embryoblast and the blastocele is an outer layer of cells called the trophoblast. At this point, it gradually loses the corona radiata and zona pellucida. When the blastocyst enters the uterus, it contains 100-150 cells.
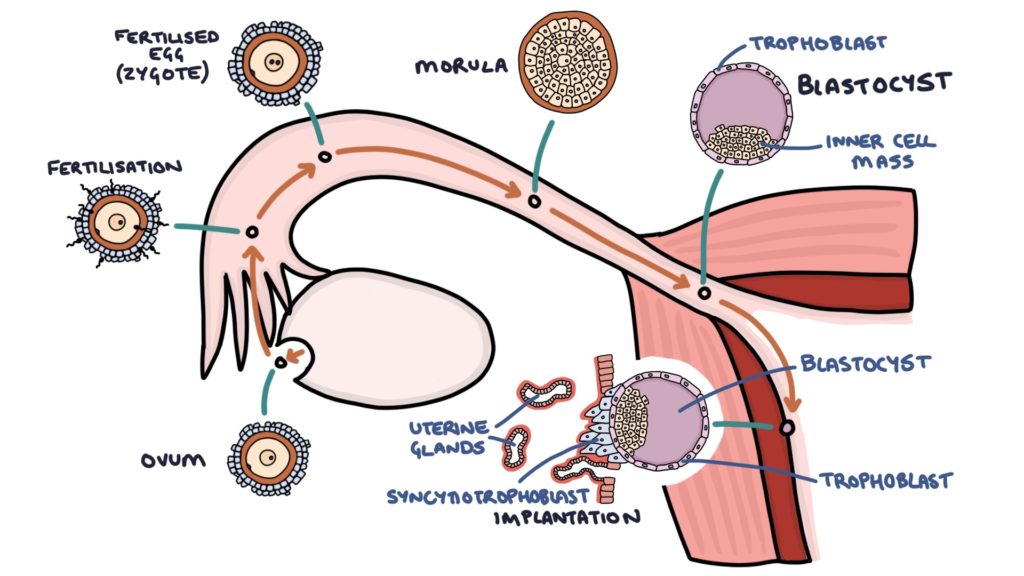
Implantation
When the blastocyst arrives at the uterus, 8 – 10 days after ovulation, it reaches the endometrium. The cells of the trophoblast (the outer layer of the blastocyst) undergo adhesion to the stroma (supportive outer tissue) of the endometrium. The outer layer of the trophoblast is called the syncytiotrophoblast. This layer forms projections into the stroma. The cells of the syncytiotrophoblast mix with the cells of the endometrium (stroma).
The cells of the stroma convert into a tissue called decidua that is specialised in providing nutrients to the trophoblast. When the blastocyst implants on the endometrium, the syncytiotrophoblast starts to produce human chorionic gonadotropin (HCG). This HCG is very important for maintaining the corpus luteum in the ovary, allowing it to continue producing progesterone and oestrogen.
Last updated May 2020
