Vasculitis describes inflammation of the blood vessels. Various specific diseases cause vasculitis, categorised based on whether they affect small, medium-sized, or large vessels.
|
Vasculitis |
Vessels |
Lab Findings |
Key Features |
|
Henoch-Schonlein Purpura |
Small |
– |
Purpura (non-blanching rash) IgA nephritis |
|
Microscopic Polyangiitis |
Small |
p-ANCA |
Glomerulonephritis Diffuse alveolar haemorrhage |
|
Granulomatosis with Polyangiitis |
Small |
c-ANCA |
Nasal symptoms Respiratory symptoms Glomerulonephritis |
|
Eosinophilic Granulomatosis with Polyangiitis |
Small |
p-ANCA Raised eosinophils |
Late-onset asthma Sinusitis and rhinitis |
|
Polyarteritis Nodosa |
Medium |
– |
Renal impairment Hypertension Cardiovascular events Tender skin nodules |
|
Kawasaki Disease |
Medium |
– |
High fever (more than 5 days) Widespread rash Bilateral conjunctivitis Strawberry tongue Coronary artery aneurysms |
|
Giant Cell Arteritis |
Large |
Raised ESR |
Unilateral headache Scalp tenderness Vision loss |
|
Takayasu’s Arteritis |
Large |
– |
Aortic arch affected “Pulseless” disease |
Presentation
There are generic vasculitis features and features more specific to individual types. Common features include:
- Joint and muscle pain
- Peripheral neuropathy
- Renal impairment
- Purpura (purple-coloured non-blanching spots caused by blood leaking from the vessels under the skin)
- Necrotic skin ulcers
- Gastrointestinal symptoms (e.g., diarrhoea, abdominal pain and bleeding)
Patients with vasculitis may also have associated systemic symptoms, including:
- Fatigue
- Fever
- Night sweats
- Weight loss
- Anorexia (loss of appetite)
- Anaemia
Investigations
Inflammatory markers (e.g., CRP and ESR) are usually raised with vasculitis.
Anti-neutrophil cytoplasmic antibodies (ANCA) are associated with specific types of vasculitis:
- p-ANCA (or MPO antibodies) – microscopic polyangiitis and eosinophilic granulomatosis with polyangiitis
- c-ANCA (or PR3 antibodies) – granulomatosis with polyangiitis
TOM TIP: The three types of vasculitis with polyangiitis in the name are associated with anti-neutrophil cytoplasmic antibodies (ANCA). Poly- refers to multiple, angi- relates to blood vessels and -itis refers to inflammation. Microscopic polyangiitis, granulomatosis with polyangiitis and eosinophilic granulomatosis with polyangiitis are types of small-vessel vasculitis. They can all affect the lungs and kidneys.
Management
The management of vasculitis depends on the type and is guided by a specialist rheumatologist. Treatment usually involves steroids and immunosuppressants.
Steroids may be administered to target the affected area:
- Oral (e.g., prednisolone)
- Intravenous (e.g., hydrocortisone)
- Nasal for nasal symptoms (e.g., granulomatosis with polyangiitis)
- Inhaled for lung involvement (e.g., eosinophilic granulomatosis with polyangiitis)
Other notable options include:
- Cyclophosphamide
- Rituximab
Henoch-Schonlein Purpura
Henoch-Schonlein purpura (HSP) is an IgA vasculitis that commonly presents in children with a purpuric rash affecting the lower limbs and buttocks. Inflammation occurs due to immunoglobulin A deposits in the blood vessels.
It affects the skin, kidneys and gastrointestinal tract. An upper airway infection or gastroenteritis often triggers the condition. It is most common in children under the age of 10 years.
The four classic features are:
- Purpura (100%),
- Joint pain (75%),
- Abdominal pain (50%)
- Renal involvement (IgA nephritis) (50%)
Management is primarily supportive, with analgesia, rest and good hydration. The use of steroids is debatable. They are monitored closely, with repeated:
- Urine dipstick monitoring for renal involvement
- Blood pressure monitoring for hypertension
Patients without kidney involvement typically recover within 4-6 weeks. A third have a recurrence of the disease within 6 months. A tiny proportion develops end-stage renal failure.
Microscopic Polyangiitis
Microscopic polyangiitis is a small vessel vasculitis. The main feature is renal failure caused by glomerulonephritis. It can also affect the lungs with diffuse alveolar haemorrhage, causing haemoptysis (coughing up blood).
Granulomatosis with Polyangiitis
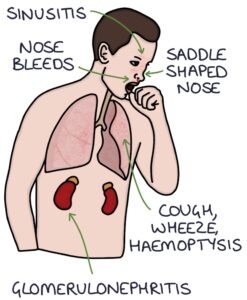
Granulomatosis with polyangiitis was previously called Wegener’s granulomatosis. It is a small-vessel vasculitis that primarily affects the respiratory tract and kidneys.
In the upper respiratory tract, it commonly affects the:
- Nose, causing nose bleeds (epistaxis), crusting in the nose and nasal secretions
- Ears, causing hearing loss
- Sinuses, causing sinusitis
A classic sign is a saddle-shaped nose due to nasal bridge collapse, causing the nasal ridge to dip inwards.
In the lower respiratory tract, it can cause cough, wheeze and haemoptysis. In the kidneys, it can cause a rapidly progressing glomerulonephritis.
Eosinophilic Granulomatosis with Polyangiitis
Eosinophilic granulomatosis with polyangiitis was previously called Churg-Strauss syndrome. It is a small-vessel vasculitis that primarily affects the lungs and skin but can affect other organs, such as the kidneys.
It typically presents with severe asthma in middle age (but can present as early as the teenage years). There may also be sinusitis and allergic rhinitis. Raised eosinophils on the full blood count is a characteristic finding.
Polyarteritis Nodosa
Polyarteritis nodosa (PAN) is a medium-vessel vasculitis. It can be idiopathic or secondary to infections, particularly hepatitis B. Typical features include:
- Renal impairment
- Hypertension
- Tender, erythematous skin nodules (similar to erythema nodosum)
- Myocardial infarction
- Stroke
- Mesenteric arteritis causing intestinal symptoms
Kawasaki Disease
Kawasaki disease is a medium-vessel vasculitis. It affects young children, typically under 5 years of age. There is no clear cause. Clinical features include:
- Persistent high fever for more than 5 days
- Widespread erythematous maculopapular rash
- Desquamation (skin peeling) of palms and soles
- Bilateral conjunctivitis
- Strawberry tongue (red tongue with prominent papillae)
A key complication is coronary artery aneurysms. Treatment is with aspirin and IV immunoglobulins.
Takayasu’s Arteritis
Takayasu’s arteritis is a form of large vessel vasculitis. It mainly affects the aorta and its branches. It can also affect the pulmonary arteries. These vessels can swell and form aneurysms or become narrowed and blocked. Stenosis or occlusion can reduce the pulses and blood pressure in a limb, leading to the name of “pulseless disease”.
It usually presents before age 40, with non-specific systemic symptoms, such as fever, malaise and muscle aches. There may be claudication symptoms (pain and fatigue that worsen while using the affected limb), particularly in an arm. Diagnosis involves CT or MRI angiography.
Last updated September 2023
Now, head over to members.zerotofinals.com and test your knowledge of this content. Testing yourself helps identify what you missed and strengthens your understanding and retention.

