Systemic lupus erythematosus (SLE) is an inflammatory autoimmune connective tissue disorder. It is “systemic” because it affects multiple organs and systems. “Erythematosus” refers to the typical red malar rash across the face.
SLE can affect anyone but occurs more commonly in:
- Women
- Asian, African, Caribbean and Hispanic ethnicity
- Young to middle-aged adults
SLE typically takes a relapsing-remitting course, with flares of worse symptoms and periods where symptoms settle. The result of chronic inflammation means SLE can shorten life expectancy (although this is mitigated with effective management). Cardiovascular disease and infection are significant complications.
Pathophysiology
SLE is characterised by anti-nuclear antibodies (ANA). These are autoantibodies against proteins within the cell nucleus. These antibodies generate a chronic inflammatory response, leading to the condition’s features.
Presentation
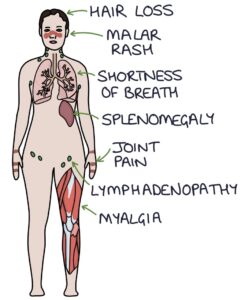
SLE presents with many non-specific symptoms:
- Fatigue
- Weight loss
- Arthralgia (joint pain)
- Non-erosive arthritis
- Myalgia (muscle pain)
- Fever
- Photosensitive malar rash
- Lymphadenopathy
- Splenomegaly
- Shortness of breath
- Pleuritic chest pain
- Mouth ulcers
- Hair loss
- Raynaud’s phenomenon
- Oedema (due to nephritis)
The typical malar rash is “butterfly” shaped across the nose and cheeks. It is triggered or worsened by sunlight.
Investigations
Abnormal investigation findings in SLE include:
- Autoantibodies (more information below)
- Full blood count may show anaemia of chronic disease, low white cell count and low platelets
- CRP and ESR may be raised with active inflammation
- C3 and C4 levels may be decreased in active disease
- Urinalysis and urine protein:creatinine ratio shows proteinuria in lupus nephritis
- Renal biopsy may be used to investigate for lupus nephritis
Autoantibodies
Around 85% of patients with SLE will be positive for anti-nuclear antibodies (ANA). These can be positive in healthy individuals and those with other autoimmune conditions (e.g., autoimmune hepatitis). A positive result needs to be interpreted in the context of their symptoms.
Anti-double stranded DNA (anti-dsDNA) antibodies are highly specific to SLE, meaning a positive result suggests SLE rather than other causes. Around half of patients with SLE have anti-dsDNA antibodies. The levels vary with disease activity, making them helpful in monitoring disease activity and response to treatment.
An extractable nuclear antigen panel looks for antibodies to specific proteins in the cell nucleus and helps diagnose and distinguish between specific connective tissue disorders:
- Anti-Sm (highly specific to SLE but not very sensitive)
- Anti-centromere antibodies (most associated with limited cutaneous systemic sclerosis)
- Anti-Ro and anti-La (most associated with Sjögren’s syndrome)
- Anti-Scl-70 (most associated with systemic sclerosis)
- Anti-Jo-1 (most associated with dermatomyositis)
Antiphospholipid antibodies and antiphospholipid syndrome can occur secondary to SLE in up to 40% of patients. These antibodies are associated with an increased risk of venous thromboembolism.
Diagnostic Criteria
The European League Against Rheumatism (EULAR) / American College of Rheumatology (ACR) criteria (2019) can be used for diagnosis. This takes into account the clinical features and autoantibodies suggestive of SLE.
Complications
Cardiovascular disease is a leading cause of death. Chronic inflammation in blood vessels leads to hypertension and coronary artery disease.
Infection is more common, both from the disease process and secondary to immunosuppressant drugs.
Anaemia in SLE can be due to anaemia of chronic disease, autoimmune haemolytic anaemia, bone marrow suppression by medications or kidney disease. It can also cause leucopenia (low white cells), neutropenia (low neutrophils) and thrombocytopenia (low platelets).
Pericarditis (inflammation of the pericardial sac surrounding the heart) causes sharp chest pain that gets worse on lying flat.
Pleuritis (inflammation of the lining of the lungs) causes sharp chest pain on inspiration.
Interstitial lung disease can be caused by inflammation in the lung tissue, leading to pulmonary fibrosis.
Lupus nephritis (inflammation in the kidney) can progress to end-stage renal failure. Investigations include a urine protein:creatinine ratio and renal biopsy. The renal biopsy is often repeated to assess the response to treatment.
Neuropsychiatric SLE is caused by inflammation in the central nervous system. It can present with optic neuritis (inflammation of the optic nerve), transverse myelitis (inflammation of the spinal cord) or psychosis.
Recurrent miscarriage is more common in SLE. There is also an increased risk of intrauterine growth restriction, pre-eclampsia and pre-term labour.
Venous thromboembolism may be associated with antiphospholipid syndrome occurring secondary to SLE.
Management
Treatment aims to control symptoms and reduce complications with the least medications and side effects. Suncream and sun avoidance are essential measures in managing the photosensitive malar rash.
First-line options include:
- Hydroxychloroquine
- NSAIDs
- Steroids (e.g., prednisolone)
Treatment options for resistant or more severe SLE include:
- DMARDs (e.g., methotrexate, mycophenolate mofetil or cyclophosphamide)
- Biologic therapies
Biological therapies include:
- Rituximab (a monoclonal antibody that targets the CD20 protein on the surface of B cells)
- Belimumab (a monoclonal antibody that targets B-cell activating factor)
Last updated August 2023
Now, head over to members.zerotofinals.com and test your knowledge of this content. Testing yourself helps identify what you missed and strengthens your understanding and retention.

