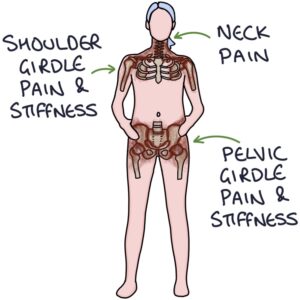
Polymyalgia rheumatica (PMR) is an inflammatory condition that causes pain and stiffness in the shoulders, pelvic girdle and neck. There is a strong association with giant cell arteritis, and the two conditions often occur together.
The cause is not fully understood. There are no relevant antibodies. It is more common in older white patients.
Presentation
Patients may have a relatively rapid onset of symptoms over days to weeks. Symptoms should be present for two weeks before a diagnosis is considered. The core symptoms are pain and stiffness of the:
- Shoulders, potentially radiating to the upper arm and elbow
- Pelvic girdle (around the hips), potentially radiating to the thighs
- Neck
The characteristic features of the pain and stiffness are:
- Worse in the morning
- Worse after rest or inactivity
- Interfere with sleep
- Take at least 45 minutes to ease in the morning
- Somewhat improve with activity

Associated features include:
- Systemic symptoms (e.g., weight loss, fatigue and low-grade fever)
- Muscle tenderness
- Carpel tunnel syndrome
- Peripheral oedema
Differential Diagnosis
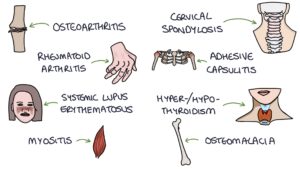
The presenting symptoms are not specific to PMR, and there is a long list of differentials, including:
- Osteoarthritis
- Rheumatoid arthritis
- Systemic lupus erythematosus
- Statin-induced myopathy
- Myositis (e.g., polymyositis)
- Cervical spondylosis
- Adhesive capsulitis (frozen shoulder)
- Hyperthyroidism or hypothyroidism
- Osteomalacia
- Fibromyalgia
- Lymphoma or leukaemia
- Myeloma
Diagnosis
Diagnosis is based on clinical presentation, response to steroids and excluding differentials.
Inflammatory markers (e.g., ESR and CRP) are usually raised (but may be normal).
The NICE clinical knowledge summaries (updated January 2023) advise investigations before initiating steroids:
- Full blood count
- Renal profile (U&E)
- Liver function tests
- Calcium (abnormal in hyperparathyroidism, cancer and osteomalacia)
- Serum protein electrophoresis for myeloma
- Thyroid-stimulating hormone for thyroid function
- Creatine kinase for myositis
- Rheumatoid factor for rheumatoid arthritis
- Urine dipstick
Additional investigations to consider:
- Anti-nuclear antibodies (ANA) for systemic lupus erythematosus
- Anti-cyclic citrullinated peptide (anti-CCP) for rheumatoid arthritis
- Urine Bence Jones protein for myeloma
- Chest x-ray for lung and mediastinal abnormalities (e.g., lung cancer or lymphoma)
Treatment
Treatment of PMR is with steroids. The NICE clinical knowledge summaries (updated January 2023) recommend:
- 15mg prednisolone daily initially
- Follow up after 1 week

Patients with PMR have a dramatic improvement in symptoms (at least 70%) within one week. Inflammatory markers return to normal within one month. A poor response to steroids suggests an alternative diagnosis.
Treatment with steroids typically lasts 1-2 years. NICE suggest the following reducing regime of prednisolone:
- 15mg until the symptoms are fully controlled, then
- 12.5mg for 3 weeks, then
- 10mg for 4-6 weeks, then
- Reducing by 1mg every 4-8 weeks
The reducing regime can go faster or slower depending on the individual and their symptom control.
Additional management for patients on long-term steroids can be remembered with the “Don’t STOP” mnemonic:
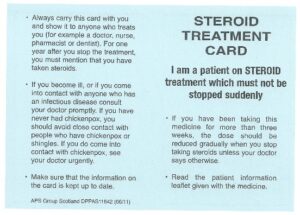
- Don’t – steroid dependence occurs after 3 weeks of treatment, and abruptly stopping risks adrenal crisis
- S – Sick day rules (steroid doses may need to be increased if the patient becomes unwell)
- T – Treatment card – patients should carry a steroid treatment card to alert others that they are steroid-dependent
- O – Osteoporosis prevention may be required (e.g., bisphosphonates and calcium and vitamin D)
- P – Proton pump inhibitors are considered for gastro-protection (e.g., omeprazole)
Last updated August 2023
