Osteoarthritis is often described as “wear and tear” in the joints. It occurs in the synovial joints and results from genetic factors, overuse and injury. Osteoarthritis is thought to result from an imbalance between cartilage damage and the chondrocyte response, leading to structural issues in the joint. Risk factors include obesity, age, occupation, trauma, being female and family history.
Commonly Affected Joints
- Hips
- Knees
- Distal interphalangeal (DIP) joints in the hands
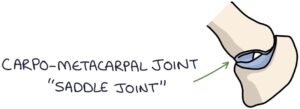
- Carpometacarpal (CMC) joint at the base of the thumb
- Lumbar spine
- Cervical spine (cervical spondylosis)
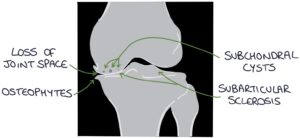
X-ray Changes
The four key x-ray changes in osteoarthritis can be remembered with the “LOSS” mnemonic:
- L – Loss of joint space
- O – Osteophytes (bone spurs)
- S – Subarticular sclerosis (increased density of the bone along the joint line)
- S – Subchondral cysts (fluid-filled holes in the bone)
X-ray reports might describe findings of osteoarthritis as degenerative changes. X-ray changes do not necessarily correlate with symptoms. A patient might have significant signs on an x-ray but minimal symptoms, or the reverse.
Presentation
Osteoarthritis presents with joint pain and stiffness. The pain and stiffness tend to worsen with activity and at the end of the day. This is the reverse of the pattern in inflammatory arthritis, where symptoms are worse in the morning and improve with activity. Osteoarthritis leads to deformity, instability and reduced function of the joint.
General signs of osteoarthritis are:
- Bulky, bony enlargement of the joint
- Restricted range of motion
- Crepitus on movement
- Effusions (fluid) around the joint
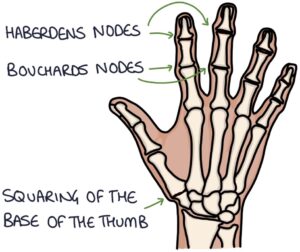
Signs in the Hands
- Heberden’s nodes (in the DIP joints)
- Bouchard’s nodes (in the PIP joints)
- Squaring at the base of the thumb (CMC joint)
- Weak grip
- Reduced range of motion
The carpometacarpal joint at the base of the thumb is a saddle joint, with the metacarpal bone sitting on the trapezius bone, using it like a saddle. It gets a lot of use and is very prone to wear.
TOM TIP: Patients may present with referred pain, particularly in the adjacent joints. For example, consider osteoarthritis in the hip in patients presenting with lower back or knee pain.
Diagnosis
The NICE guidelines (2022) suggest that a diagnosis can be made without any investigations if the patient is over 45, has typical pain associated with activity and has no morning stiffness (or stiffness lasting under 30 minutes).
Management
Non-pharmacological management involves patient education and lifestyle changes, such as:
- Therapeutic exercise to improve strength and function and reduce pain
- Weight loss if overweight, to reduce the load on the joint
- Occupational therapy to support activities and function (e.g., walking aids and adaptations to the home)
Pharmacological management recommended by the NICE guidelines (2022) are:
- Topical NSAIDs first-line for knee osteoarthritis
- Oral NSAIDs where required and suitable (co-prescribed with a proton pump inhibitor for gastroprotection)
Weak opiates and paracetamol are only recommended for short-term, infrequent use. NICE (2022) recommend against using any strong opiates for osteoarthritis.
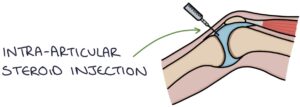
Intra-articular steroid injections may temporarily improve symptoms (NICE say up to 10 weeks).
Joint replacement may be used in severe cases. The hips and knees are the most commonly replaced joints.
Medication Notes
NSAIDs (e.g., ibuprofen or naproxen) are very effective for musculoskeletal pain. However, they must be used cautiously, particularly in older patients and those on anticoagulants, such as aspirin or DOACs. They are best used intermittently, only for a short time during flares. They have several potential adverse effects, including:
- Gastrointestinal side effects, such as gastritis and peptic ulcers (leading to upper gastrointestinal bleeding)
- Renal side effects, such as acute kidney injury (e.g., acute tubular necrosis) and chronic kidney disease
- Cardiovascular side effects, such as hypertension, heart failure, myocardial infarction and stroke
- Exacerbating asthma
There is little evidence that opiates help with chronic pain. They are associated with side effects, risks, tolerance, dependence and withdrawal. They often result in dependence without any objective benefits.
TOM TIP: The WHO pain ladder is not helpful in chronic pain. Paracetamol and opiates are not recommended for regular use in osteoarthritis. Remember that NSAIDs cause hypertension by blocking prostaglandins (prostaglandins cause vasodilation) and should be used very cautiously with a history of high blood pressure.
Last updated August 2023
