Giant cell arteritis (GCA) is also known as temporal arteritis. It is a type of systemic vasculitis affecting the medium and large arteries. There is a strong link with polymyalgia rheumatica. It is more common in older white patients.
The key complication of giant cell arteritis is vision loss, which is often irreversible.
Presentation
Unilateral headache is the primary presenting feature, typically severe and around the temple and forehead. It may be associated with:
- Scalp tenderness (e.g., noticed when brushing the hair)
- Jaw claudication
- Blurred or double vision
- Loss of vision if untreated
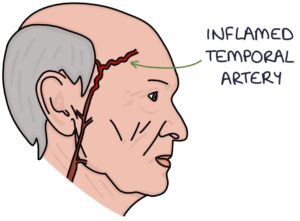
The temporal artery may be tender and thickened to palpation, with reduced or absent pulsation.
Associated features include:
- Symptoms of polymyalgia rheumatica (e.g., shoulder and pelvic girdle pain and stiffness)
- Systemic symptoms (e.g., weight loss, fatigue and low-grade fever)
- Muscle tenderness
- Carpel tunnel syndrome
- Peripheral oedema
Diagnosis
The diagnosis is based on:
- Clinical presentation
- Raised inflammatory markers, particularly ESR (usually more than 50 mm/hour)
- Temporal artery biopsy (showing multinucleated giant cells)
- Duplex ultrasound (showing the hypoechoic “halo” sign and stenosis of the temporal artery)
Management
Steroids are the mainstay of treatment. They are started immediately, before confirming the diagnosis, to reduce the risk of vision loss. There is usually a rapid and significant response to steroid treatment. Initial treatment is:
- 40-60mg prednisolone daily with no visual symptoms or jaw claudication
- 500mg-1000mg methylprednisolone daily with visual symptoms or jaw claudication
Once the diagnosis is confirmed and the condition is controlled, the steroid dose is slowly weaned over 1-2 years.
Other medications include:
- Aspirin 75mg daily decreases vision loss and strokes
- Proton pump inhibitor (e.g., omeprazole) for gastroprotection while on steroids
- Bisphosphonates and calcium and vitamin D for bone protection while on steroids
A combination of specialties manages patients with GCA:
- Rheumatology for specialist diagnosis and management
- Vascular surgeons for a temporal artery biopsy
- Ophthalmology review for visual symptoms
Complications
- Steroid-related complications (e.g., weight gain, diabetes and osteoporosis)
- Visual loss
- Cerebrovascular accident (stroke)
Last updated August 2023
