Pulmonary hypertension refers to increased resistance and pressure in the pulmonary arteries. It causes strain on the right side of the heart as it tries to pump blood through the lungs. There is back pressure through the right side of the heart and into the systemic venous system.
Pulmonary hypertension is defined as a mean pulmonary arterial pressure of more than 20 mmHg.
Causes
The causes of pulmonary hypertension can be classified into five groups:
- Group 1 – Idiopathic pulmonary hypertension or connective tissue disease (e.g., systemic lupus erythematous)
- Group 2 – Left heart failure, usually due to myocardial infarction or systemic hypertension
- Group 3 – Chronic lung disease (e.g., COPD or pulmonary fibrosis)
- Group 4 – Pulmonary vascular disease (e.g., pulmonary embolism)
- Group 5 – Miscellaneous causes such as sarcoidosis, glycogen storage disease and haematological disorders
Signs and Symptoms
Shortness of breath is the main presenting symptom. Other signs and symptoms include:
- Syncope (loss of consciousness)
- Tachycardia
- Raised jugular venous pressure (JVP)
- Hepatomegaly
- Peripheral oedema
Investigations
ECG changes indicate right-sided heart strain:
- P pulmonale (peaked P waves)
- Right ventricular hypertrophy (tall R waves in V1 and V2 and deep S waves in V5 and V6)
- Right axis deviation
- Right bundle branch block
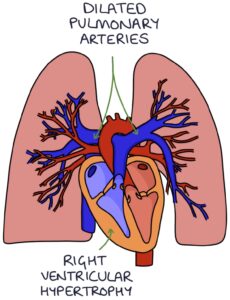
Chest x-ray changes include:
- Dilated pulmonary arteries
- Right ventricular hypertrophy
Other investigations include:
- Raised NT‑proBNP blood test result indicates right ventricular failure
- Echocardiogram can be used to estimate the pulmonary artery pressure
Management
The prognosis of idiopathic pulmonary hypertension is poor, with a mean survival of 2-3 years after the diagnosis if untreated.
Idiopathic pulmonary hypertension may be treated with:
- Calcium channel blockers
- Intravenous prostaglandins (e.g., epoprostenol)
- Endothelin receptor antagonists (e.g., macitentan)
- Phosphodiesterase-5 inhibitors (e.g., sildenafil)
Secondary pulmonary hypertension is managed by treating the underlying cause, such as pulmonary embolism, COPD or systemic lupus erythematosus.
Supportive treatments (e.g., oxygen and diuretics) are used for complications such as respiratory failure, oedema and arrhythmias.
Last updated June 2023
Now, head over to members.zerotofinals.com and test your knowledge of this content. Testing yourself helps identify what you missed and strengthens your understanding and retention.

