A pleural effusion is a collection of fluid in the pleural space. Pleural effusions can be broadly categorised into:
- Exudative – a high protein content (more than 30g/L)
- Transudative – a lower protein content (less than 30g/L)
Light’s criteria are used for establishing an exudative effusion using protein or lactate dehydrogenase (LDH):
- Pleural fluid protein / serum protein greater than 0.5
- Pleural fluid LDH / serum LDH greater than 0.6
- Pleural fluid LDH greater than 2/3 of the normal upper limit of the serum LDH
Causes
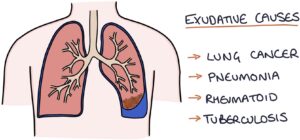
Exudative causes are related to inflammation. The inflammation results in protein leaking out of the tissues into the pleural space (ex- meaning moving out of). The top causes are:
- Cancer (e.g., lung cancer or mesothelioma)
- Infection (e.g., pneumonia or tuberculosis)
- Rheumatoid arthritis
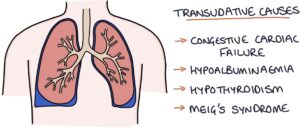
Transudative causes relate to fluid moving across or shifting into the pleural space (trans- meaning moving across):
- Congestive cardiac failure
- Hypoalbuminaemia
- Hypothyroidism
- Meigs syndrome
TOM TIP: Meigs syndrome involves a triad of a benign ovarian tumour (usually a fibroma), pleural effusion and ascites. This often appears in exams. The pleural effusion and ascites resolve with the removal of the tumour.
Presentation
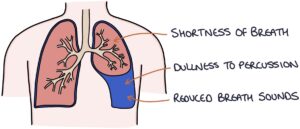
The typical presenting symptom is shortness of breath.
Examination findings are:
- Dullness to percussion over the effusion
- Reduced breath sounds
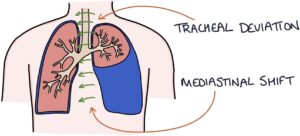
- Tracheal deviation away from the effusion in very large effusions
Investigations
Chest x-ray findings are:
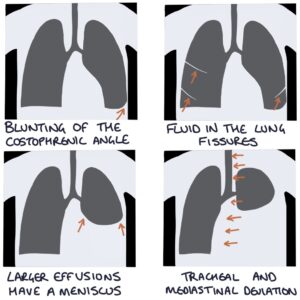
- Blunting of the costophrenic angle
- Fluid in the lung fissures
- Larger effusions will have a meniscus (a curving upwards where it meets the chest wall and mediastinum)
- Tracheal and mediastinal deviation away from the effusion in very large effusions
Ultrasound and CT can detect smaller effusions than a chest x-ray, estimate the volume and identify potential causes.
Pleural fluid analysis requires a sample taken by aspiration or chest drain. This helps establish the underlying cause by measuring the protein content, LDH, cell count, pH, glucose and microbiology testing.
Treatment
Diagnosing and treating the underlying cause is the mainstay of management.
Conservative management may be appropriate as small effusions will resolve with treatment of the underlying cause. More significant effusions often need aspiration or drainage.
Pleural aspiration involves sticking a needle through the chest wall into the effusion and aspirating the fluid. Aspiration can temporarily relieve the pressure, but the effusion may recur, and further drainage may be required.
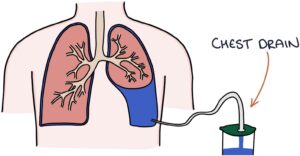
Chest drain can be used to drain the effusion and prevent it from recurring.
Empyema
Empyema refers to an infected pleural effusion. Suspect an empyema in a patient with improving pneumonia but a new or ongoing fever. Pleural aspiration shows pus, low pH, low glucose and high LDH. Empyema is treated with a chest drain and antibiotics.
Last updated June 2023