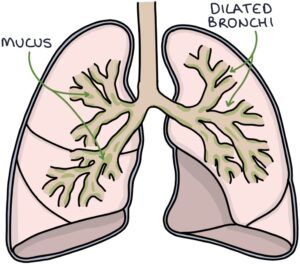
Bronchiectasis involves permanent dilation of the bronchi, the large airways that transport air to the lungs. Sputum collects and organisms grow in the wide tubes, resulting in a chronic cough, continuous sputum production and recurrent infections.
Bronchiectasis results from damage to the airways. Potential causes of this damage include:
- Idiopathic (no apparent cause)
- Pneumonia
- Whooping cough (pertussis)
- Tuberculosis
- Alpha-1-antitrypsin deficiency
- Connective tissue disorders (e.g., rheumatoid arthritis)
- Cystic fibrosis
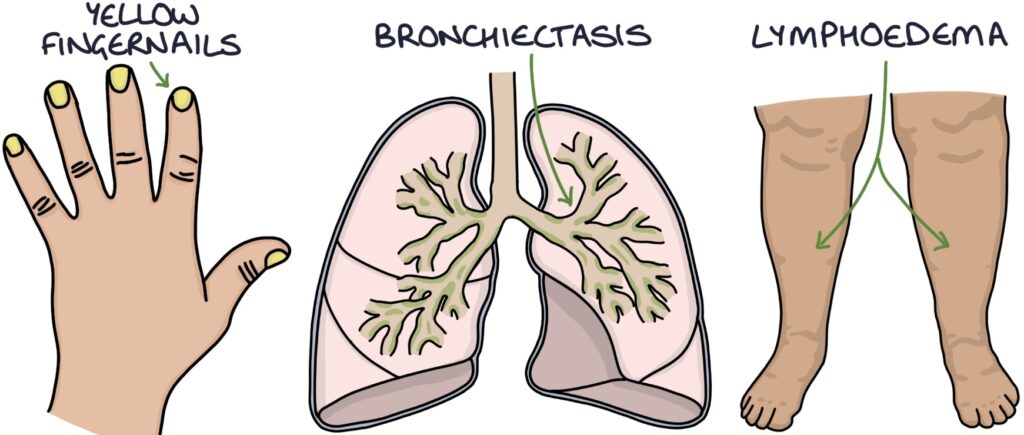
- Yellow nail syndrome
TOM TIP: Yellow nail syndrome is characterised by yellow fingernails, bronchiectasis and lymphoedema. Patients are stable and have good clinical signs, making it a good choice for OSCEs. As it is rare, examiners will score high marks if you can combine these features and name the diagnosis.
Symptoms
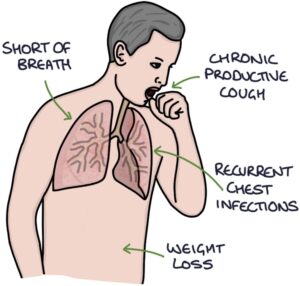
Key presenting symptoms are:
- Shortness of breath
- Chronic productive cough
- Recurrent chest infections
- Weight loss
Signs
Signs of bronchiectasis on examination include:
- Sputum pot by the bedside
- Oxygen therapy (if needed)
- Weight loss (cachexia)
- Finger clubbing
- Signs of cor pulmonale (e.g., raised JVP and peripheral oedema)
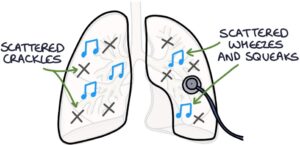
- Scattered crackles throughout the chest that change or clear with coughing
- Scattered wheezes and squeaks
Investigations
Sputum culture is used to identify colonising and infective organisms. The most common infective organisms are:
- Haemophilus influenza
- Pseudomonas aeruginosa
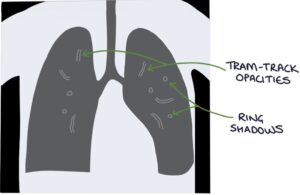
Chest x-ray findings include:
- Tram-track opacities (parallel markings of a side-view of the dilated airway)
- Ring shadows (dilated airways seen end-on)
High-resolution CT (HRCT) is the test of choice for establishing the diagnosis.
Management
General management involves:
- Vaccines (e.g., pneumococcal and influenza)
- Respiratory physiotherapy to help clear sputum
- Pulmonary rehabilitation
- Long-term antibiotics (e.g., azithromycin) for frequent exacerbations (e.g., 3 or more per year)
- Inhaled colistin for Pseudomonas aeruginosa colonisation
- Long-acting bronchodilators may be considered for breathlessness
- Long-term oxygen therapy in patients with reduced oxygen saturation
- Surgical lung resection may be considered for specific areas of disease
- Lung transplant is an option for end-stage disease
Infective exacerbations require:
- Sputum culture (before antibiotics)
- Extended courses of antibiotics, usually 7–14 days
- Ciprofloxacin is the usual choice for exacerbations caused by Pseudomonas aeruginosa
TOM TIP: The key features to remember with bronchiectasis are finger clubbing, diagnosis by HRCT, Pseudomonas colonisation and extended courses of 7-14 days of antibiotics for exacerbations.
Last updated September 2023
Now, head over to members.zerotofinals.com and test your knowledge of this content. Testing yourself helps identify what you missed and strengthens your understanding and retention.

