Haemolytic uraemic syndrome (HUS) involves thrombosis in small blood vessels throughout the body, usually triggered by Shiga toxins from either E. coli O157 or Shigella.

It most often affects children following an episode of gastroenteritis. Antibiotics and anti-motility medication (e.g., loperamide) used to treat gastroenteritis caused by E. coli O157 or Shigella increase the risk of HUS.
HUS leads to the classic triad of:
- Microangiopathic haemolytic anaemia
- Acute kidney injury
- Thrombocytopenia (low platelets)
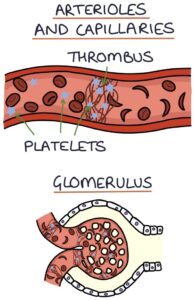
The formation of blood clots consumes platelets, leading to thrombocytopenia. The blood flow through the kidney is affected by thrombi and damaged red blood cells, leading to acute kidney injury.
Microangiopathic haemolytic anaemia (MAHA) involves the destruction of red blood cells (haemolysis) due to pathology in the small vessels (microangiopathy). Tiny blood clots (thrombi) partially obstruct the small blood vessels and churn the red blood cells as they pass through, causing them to rupture.
Presentation
E. coli O157 and Shigella cause gastroenteritis. Diarrhoea is the first symptom, which turns bloody within 3 days. Around a week after the onset of diarrhoea, the features of HUS develop:
- Fever
- Abdominal pain
- Lethargy
- Pallor
- Reduced urine output (oliguria)
- Haematuria
- Hypertension
- Bruising
- Jaundice (due to haemolysis)
- Confusion

Management
Stool culture is used to establish the causative organism.
HUS is a medical emergency and requires hospital admission and supportive management with treatment of:
- Hypovolaemia (e.g., IV fluids)
- Hypertension
- Severe anaemia (e.g., blood transfusions)
- Severe renal failure (e.g., haemodialysis)
It is self-limiting, and most patients fully recover with good supportive care.
Last updated September 2023
Now, head over to members.zerotofinals.com and test your knowledge of this content. Testing yourself helps identify what you missed and strengthens your understanding and retention.

