Acute kidney injury (AKI) refers to a rapid drop in kidney function, diagnosed by measuring the serum creatinine. Acute kidney injury is most common in acutely unwell patients (e.g., infections or following surgery).
The NICE guidelines (2019) criteria for diagnosing an acute kidney injury are:
- Rise in creatinine of more than 25 micromol/L in 48 hours
- Rise in creatinine of more than 50% in 7 days
- Urine output of less than 0.5 ml/kg/hour over at least 6 hours
Risk Factors
Risk factors that would predispose to developing acute kidney injury include:
- Older age (e.g., above 65 years)
- Sepsis
- Chronic kidney disease
- Heart failure
- Diabetes
- Liver disease
- Cognitive impairment (leading to reduced fluid intake)
- Medications (e.g., NSAIDs, gentamicin, diuretics and ACE inhibitors)
- Radiocontrast agents (e.g., used during CT scans)
Causes
TOM TIP: Whenever someone asks you the causes of renal impairment, start with, “the causes are pre-renal, renal or post-renal”. This will impress them and allow you to think through the causes more logically.
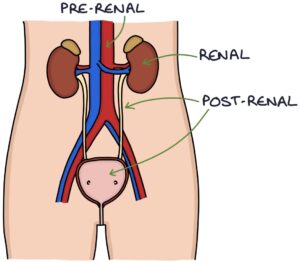
Pre-renal causes are the most common. Insufficient blood supply (hypoperfusion) to kidneys reduces the filtration of blood. This may be due to:
- Dehydration
- Shock (e.g., sepsis or acute blood loss)
- Heart failure
Renal causes are due to intrinsic disease in the kidney. This may be due to:
- Acute tubular necrosis
- Glomerulonephritis
- Acute interstitial nephritis
- Haemolytic uraemic syndrome
- Rhabdomyolysis
Post-renal causes involve obstruction to the outflow of urine away from the kidney, causing back-pressure into the kidney and reduced kidney function. This is called an obstructive uropathy. Obstruction may be caused by:
- Kidney stones
- Tumours (e.g., retroperitoneal, bladder or prostate)
- Strictures of the ureters or urethra
- Benign prostatic hyperplasia (benign enlarged prostate)
- Neurogenic bladder
Acute Tubular Necrosis
Acute tubular necrosis refers to damage and death (necrosis) of the epithelial cells of the renal tubules. It is the most common intrinsic cause of acute kidney injury. Damage to the kidney cells occurs due to:
- Ischaemia due to hypoperfusion (e.g., dehydration, shock or heart failure)
- Nephrotoxins (e.g., gentamicin, radiocontrast agents or cisplatin)
Muddy brown casts on urinalysis confirm acute tubular necrosis. Renal tubular epithelial cells may also be seen.
The epithelial cells can regenerate, making acute tubular necrosis reversible. Recovery usually takes 1-3 weeks.
Acute Interstitial Nephritis
Acute interstitial nephritis (AIN) is a common cause of acute kidney injury. It involves acute inflammation of the interstitium (the space between the tubules and vessels). It is caused by an immune reaction associated with:
- Drugs (e.g. NSAIDs or antibiotics)
- Infections (e.g., E. coli or HIV)
- Autoimmune conditions (e.g., sarcoidosis or SLE)
Other features can accompany the acute kidney injury, specifically:
- Rash
- Fever
- Flank pain
- Eosinophilia
Management involves treating the underlying cause. Steroids may reduce inflammation and improve recovery.
Investigations
Urinalysis assesses for protein, blood, leucocytes, nitrites and glucose:
- Leucocytes and nitrites suggest infection
- Protein and blood suggest acute nephritis (but can be positive in infection)
- Glucose suggests diabetes
Ultrasound of the urinary tract assesses for obstruction when a post-renal cause is suspected.
Management
Acute kidney injury is often preventable by:
- Avoiding nephrotoxic medications where appropriate
- Ensuring adequate fluid intake (including IV fluids if oral intake is inadequate)
- Additional fluids before and after radiocontrast agents
Treating an acute kidney injury involves reversing the underlying cause and supportive management, for example:
- IV fluids for dehydration and hypovolaemia
- Withhold medications that may worsen the condition (e.g., NSAIDs and ACE inhibitors)
- Withhold/adjust medications that may accumulate with reduced renal function (e.g., metformin and opiates)
- Relieve the obstruction in a post-renal AKI (e.g., insert a catheter in a patient with prostatic hyperplasia)
- Dialysis may be required in severe cases
Input from a renal specialist is required where there is severe AKI, doubt about the cause or complications.
TOM TIP: Calling ACE inhibitors nephrotoxic is incorrect. ACE inhibitors should be stopped in an acute kidney injury, as they reduce the filtration pressure. However, ACE inhibitors have a protective effect on the kidneys long-term. They are offered to certain patients with hypertension, diabetes and chronic kidney disease to protect the kidneys from further damage.
Complications
- Fluid overload, heart failure and pulmonary oedema
- Hyperkalaemia
- Metabolic acidosis
- Uraemia (high urea), which can lead to encephalopathy and pericarditis
Last updated September 2023
Now, head over to members.zerotofinals.com and test your knowledge of this content. Testing yourself helps identify what you missed and strengthens your understanding and retention.

