Retinal vein occlusion occurs when a blood clot (thrombus) forms in the retinal veins, blocking the drainage of blood from the retina. The thrombus may form in the central retinal vein or branch retinal veins.
The branch retinal veins drain into the central retinal vein, which runs through the optic nerve to drain into either the superior ophthalmic vein or cavernous sinus. Blockage of one of the branch veins affects the area drained by that branch. Blockage in the central vein causes problems with the whole retina.
Sites where the retinal arteries cross over the top of the veins can cause narrowing of the vein. These sites are at higher risk of occlusion.
Blockage of a retinal vein causes venous congestion in the retina. Increased pressure in the retinal veins results in fluid and blood leaking into the retina, causing macular oedema and retinal haemorrhages. This results in retinal damage and vision loss.
Retinal vein occlusion can be categorised as ischaemic or non-ischaemic. Retinal ischaemia leads to the release of vascular endothelial growth factor (VEGF), resulting in new blood vessel development (neovascularisation).
Risk Factors
- Hypertension
- High cholesterol
- Diabetes
- Smoking
- High plasma viscosity (e.g., myeloma)
- Myeloproliferative disorders
- Inflammatory conditions (e.g., SLE)
Presentation
Retinal vein occlusion causes painless blurred vision or vision loss. In branch retinal vein occlusion, the vision loss corresponds to the affected area of the retina. When it involves the branch draining the macula, central vision is lost.
Fundoscopy examination gives characteristic findings:
- Dilated tortuous retinal veins
- Flame and blot haemorrhages
- Retinal oedema
- Cotton wool spots
- Hard exudates
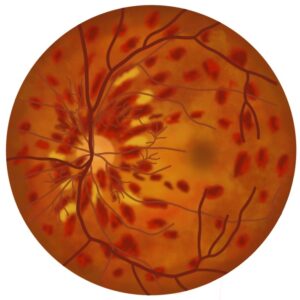
TOM TIP: The fundus in retinal vein occlusion has a characteristic “blood and thunder” appearance. It looks like someone has painted streaks of blood across the surface. The appearance may get confused with the “pizza pie” appearance of cytomegalovirus (CMV) retinitis, which occurs with CMV infection of the eye, typically in severely immunocompromised patients (commonly end-stage HIV).
Management
Patients with suspected retinal vein occlusion should be referred immediately to an ophthalmologist.
Management in secondary care aims to treat macular oedema and prevent neovascularisation. The options are:
- Anti-VEGF therapies (e.g., ranibizumab and aflibercept)
- Dexamethasone intravitreal implant (to treat macular oedema)
- Laser photocoagulation (to treat new vessels)
Last updated October 2023
