Age-related macular degeneration (AMD) is a progressive condition affecting the macula. It is the most common cause of blindness in the UK. It is often unilateral but may be bilateral. There are two types:
- Wet (also called neovascular), accounting for 10% of cases
- Dry (also called non-neovascular), accounting for 90% of cases
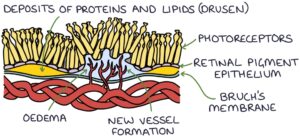
The macula is found in the centre of the retina. It generates high-definition colour vision in the central visual field. It has four layers:
- Choroid layer (at the base), which contains the blood vessels that supply the macula
- Bruch’s membrane
- Retinal pigment epithelium
- Photoreceptors (towards the surface)
Drusen are an important finding with AMD. Drusen are yellowish deposits of proteins and lipids between the retinal pigment epithelium and Bruch’s membrane. A few small drusen can be normal in older patients. Frequent and larger drusen can be an early sign of macular degeneration.
Other features that are common to wet and dry AMD are:
- Atrophy of the retinal pigment epithelium
- Degeneration of the photoreceptors
In wet AMD, new vessels develop from the choroid layer and grow into the retina (neovascularisation). These vessels can leak fluid or blood, causing oedema and faster vision loss. A key chemical that stimulates the development of new vessels is vascular endothelial growth factor (VEGF). This is the target of medications to treat wet AMD.
Risk Factors
- Older age
- Smoking
- Family history
- Cardiovascular disease (e.g., hypertension)
- Obesity
- Poor diet (low in vitamins and high in fat)
Presentation
Visual changes associated with AMD tend to be unilateral, with:
- Gradual loss of central vision
- Reduced visual acuity
- Crooked or wavy appearance to straight lines (metamorphopsia)
Patients often present with a gradually worsening ability to read small text.
Wet AMD presents more acutely than dry AMD. Vision loss can develop within days and progress to complete vision loss within 2-3 years. It often progresses to bilateral disease.
TOM TIP: Glaucoma is associated with peripheral vision loss and halos around lights. AMD is associated with central vision loss and a wavy appearance to straight lines. This helps you tell them apart in exams.
Examination
Key findings on examination are:
- Reduced visual acuity using a Snellen chart
- Scotoma (an enlarged central area of vision loss)
- Amsler grid test can be used to assess for the distortion of straight lines seen in AMD
- Drusen may be seen during fundoscopy
Slit lamp examination gives a detailed view of the retina and macula.
Optical coherence tomography gives a cross-sectional view of the layers of the retina and is used for diagnosing and monitoring AMD.
Fluorescein angiography involves giving a fluorescein contrast and photographing the retina to assess the blood supply, showing oedema and neovascularisation in wet AMD.
Management
Patients with suspected AMD require specialist ophthalmology assessment and management.
There is no specific treatment for dry AMD. Management involves monitoring and reducing the risk of progression by:
- Avoiding smoking
- Controlling blood pressure
- Vitamin supplementation has some evidence in slowing progression
Anti-VEGF medications are used to treat wet AMD (not dry AMD). Vascular endothelial growth factor (VEGF) stimulates the development of new blood vessels in the retina. Anti-VEGF medications (e.g., ranibizumab, aflibercept and bevacizumab) block VEGF and slow the development of new vessels. They are injected directly into the vitreous chamber of the eye (intravitreal), usually about once a month.
Last updated October 2023
