Stroke is also called cerebrovascular accident (CVA). Cerebrovascular accidents are either:
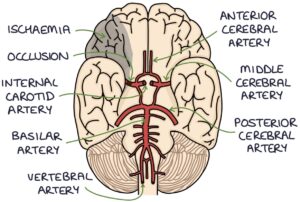
- Ischaemia or infarction of the brain tissue secondary to a disrupted blood supply (ischaemic stroke)
- Intracranial haemorrhage, with bleeding in or around the brain (haemorrhagic stroke)
Ischaemia refers to an inadequate blood supply. Infarction refers to tissue death due to ischaemia.
The blood supply to the brain may be disrupted by:
- A thrombus or embolus
- Atherosclerosis
- Shock
- Vasculitis
Transient ischaemic attack (TIA) involves temporary neurological dysfunction (lasting less than 24 hours) caused by ischaemia but without infarction. Symptoms have a rapid onset and often resolve before the patient is seen. TIAs may precede a stroke. Crescendo TIAs are two or more TIAs within a week and indicate a high risk of stroke.
Presentation
A sudden onset of neurological symptoms suggests a vascular cause (e.g., stroke). Stroke symptoms are typically asymmetrical. Common symptoms are:
- Limb weakness
- Facial weakness
- Dysphasia (speech disturbance)
- Visual field defects
- Sensory loss
- Ataxia and vertigo (posterior circulation infarction)
Risk Factors
- Previous stroke or TIA
- Atrial fibrillation
- Carotid artery stenosis
- Hypertension
- Diabetes
- Raised cholesterol
- Family history
- Smoking
- Obesity
- Vasculitis
- Thrombophilia
- Combined contraceptive pill
TOM TIP: The combined contraceptive pill carries a tiny increased risk of stroke. The risk is higher in patients with migraines with aura, smokers over 34 years or those with a history of stroke or TIA.
FAST Tool
The FAST tool is used as a simple way to identify stroke in the community:
- F – Face
- A – Arm
- S – Speech
- T – Time (act fast and call 999)
ROSIER Tool
The ROSIER tool (Recognition Of Stroke In the Emergency Room) gives a score based on the clinical features and duration. Stroke is possible in patients scoring one or more.
Management of TIA
Symptoms should have completely resolved within 24 hours of onset. Initial management involves:
- Aspirin 300mg daily (started immediately)
- Referral for specialist assessment within 24 hours (within 7 days if more than 7 days since the episode)
- Diffusion-weighted MRI scan is the imaging investigation of choice.
Management of Stroke
The information here is summarised from the NICE guidelines (updated 2022) on stroke. Initial management involves:
- Exclude hypoglycaemia
- Immediate CT brain to exclude haemorrhage
- Aspirin 300mg daily for two weeks (started after haemorrhage is excluded with a CT)
- Admission to a specialist stroke centre
Thrombolysis with alteplase is considered once haemorrhage is excluded (after the CT scan). Alteplase is a tissue plasminogen activator that rapidly breaks down clots. It may be given within 4.5 hours of the symptom onset, based on local protocols and by an appropriately trained team. Patients need close monitoring for complications, particularly intracranial or systemic haemorrhage, with access to immediate imaging if bleeding is suspected.
Thrombectomy is considered in patients with a confirmed blockage of the proximal anterior circulation or proximal posterior circulation. It may be considered within 24 hours of the symptom onset and alongside IV thrombolysis.
In patients with an ischaemic stroke, lowering the blood pressure can worsen the ischaemia. High blood pressure treatment is only indicated in hypertensive emergency or to reduce the risks when giving intravenous thrombolysis. Blood pressure is aggressively treated in patients with a haemorrhagic stroke.
Assessment for Underlying Causes
Patients with a TIA or stroke are investigated for carotid artery stenosis and atrial fibrillation with:
- Carotid imaging (e.g., carotid ultrasound, or CT or MRI angiogram)
- ECG or ambulatory ECG monitoring
Anticoagulation is initiated for atrial fibrillation (after excluding haemorrhage and finishing two weeks of aspirin).
Surgical interventions are considered where there is significant carotid artery stenosis. The options are:
- Carotid endarterectomy (recommended in the NICE guidelines)
- Angioplasty and stenting
TOM TIP: The top risk factors to remember are atrial fibrillation and carotid artery stenosis. All patients with a TIA or stroke will have carotid imaging and ECGs to identify these.
Secondary Prevention
- Clopidogrel 75mg once daily (alternatively aspirin plus dipyridamole)
- Atorvastatin 20-80mg (not started immediately – usually delayed at least 48 hours)
- Blood pressure and diabetes control
- Addressing modifiable risk factors (e.g., smoking, obesity and exercise)
Rehabilitation
Stroke patients require a period of adjustment and rehabilitation involving a multi-disciplinary team of:
- Stroke physicians
- Nurses
- Speech and language (SALT) to assess swallowing
- Dieticians in those at risk of malnutrition
- Physiotherapy
- Occupational therapy
- Social services
- Optometry and ophthalmology
- Psychology
- Orthotics
Last updated September 2023
Now, head over to members.zerotofinals.com and test your knowledge of this content. Testing yourself helps identify what you missed and strengthens your understanding and retention.

