Migraine is a complex neurological condition causing episodes or attacks of headache and associated symptoms. It is very common, tends to affect women more often than men and is most common in teenagers and young adults.
Migraine can be categorised into four main types:
- Migraine without aura
- Migraine with aura
- Silent migraine (migraine with aura but without a headache)
- Hemiplegic migraine
The pathophysiology of migraine has been studied for decades. Various mechanisms and theories have developed. It is likely a combination of structural, functional, chemical, vascular and inflammatory factors.
Typical Symptoms
There are five stages of migraine:
- Premonitory or prodromal stage (can begin several days before the headache)
- Aura (lasting up to 60 minutes)
- Headache stage (lasts 4 to 72 hours)
- Resolution stage (the headache may fade away or be relieved abruptly by vomiting or sleeping)
- Postdromal or recovery phase
These stages vary between patients. Some patients may only experience one or two of the stages. The prodromal stage may involve days of subtle symptoms (e.g., yawning, fatigue or mood change) before the headache starts.
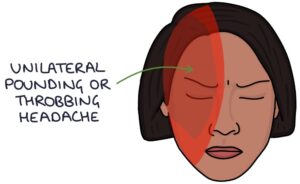
Migraine headaches last between 4 and 72 hours. Typical features are:
- Usually unilateral but can be bilateral
- Moderate-severe intensity
- Pounding or throbbing in nature
- Photophobia (discomfort with lights)
- Phonophobia (discomfort with loud noises)
- Osmophobia (discomfort with strong smells)
- Aura (visual changes)
- Nausea and vomiting
Aura
Aura can affect vision, sensation or language. Visual symptoms are the most common. These may be:
- Sparks in the vision
- Blurred vision
- Lines across the vision
- Loss of visual fields (e.g., scotoma)
Sensation changes may include tingling or numbness. Language symptoms include dysphasia (difficulty speaking).
Hemiplegic Migraine
The main feature of hemiplegic migraines is hemiplegia (unilateral limb weakness). Other symptoms may include ataxia (loss of coordination) and impaired consciousness.
Familial hemiplegic migraine is an autosomal dominant genetic condition characterised by hemiplegic migraines that run in families. However, hemiplegic migraines also occur without any genetic link or family history.
Hemiplegic migraines can mimic a stroke or TIA. It is essential to exclude a stroke with sudden-onset hemiplegia.
Triggers
Migraine triggers vary between patients and may include:
- Stress
- Bright lights
- Strong smells
- Certain foods (e.g., chocolate, cheese and caffeine)
- Dehydration
- Menstruation
- Disrupted sleep
- Trauma
Acute Management
Patients may develop strategies for managing symptoms, often retreating to a dark, quiet room and sleeping.
Medical options for an acute attack are:
- NSAIDs (e.g., ibuprofen or naproxen)
- Paracetamol
- Triptans (e.g., sumatriptan)
- Antiemetics if vomiting occurs (e.g., metoclopramide or prochlorperazine)
Opiates are not used to treat migraines and may make the condition worse.
Triptans
Triptans are used to abort migraines when they start to develop. They are 5-HT receptor agonists (they bind to and stimulate serotonin receptors), specifically 5-HT1B and 5-HT1D. They have various mechanisms of action, including:
- Cranial vasoconstriction
- Inhibiting the transmission of pain signals
- Inhibiting the release of inflammatory neuropeptides
Triptans (e.g., sumatriptan) are taken as soon as a migraine headache starts. They should halt the attack. If the attack resolves and then reoccurs, another dose can be taken. If it does not work the first time, another second dose should not be taken for the same attack.
The main contraindications relate to risks associated with vasoconstriction, for example, hypertension, coronary artery disease or previous stroke, TIA or myocardial infarction.
Prophylaxis
A headache diary can help identify the triggers and assess the response to treatment. Avoiding triggers can be helpful.
The usual prophylactic medications to reduce the frequency and severity of attacks are:
- Propranolol (a non-selective beta blocker)
- Amitriptyline (a tricyclic antidepressant)
- Topiramate (teratogenic and very effective contraception is needed)
More specialist options include:
- Pizotifen
- Candesartan
- Sodium valproate
- Monoclonal antibodies (e.g., erenumab and fremanezumab)
Other options mentioned in the NICE clinical knowledge summaries (updated 2022) include:
- Cognitive behavioural therapy
- Mindfulness and meditation
- Acupuncture
- Vitamin B2 (riboflavin)
Prophylactic triptans (e.g., frovatriptan or zolmitriptan) are an option for menstrual migraines. Symptoms tend to occur two days before until three days after the start of menstruation. Regular triptans may be taken during this time.
Migraines tend to become less frequent and severe or stop altogether with time, particularly after menopause.
Migraines are associated with a slightly increased risk of stroke, particularly when associated with aura. The risk of stroke is further increased with the combined contraceptive pill, making them a contraindication to the combined pill.
Last updated October 2023
