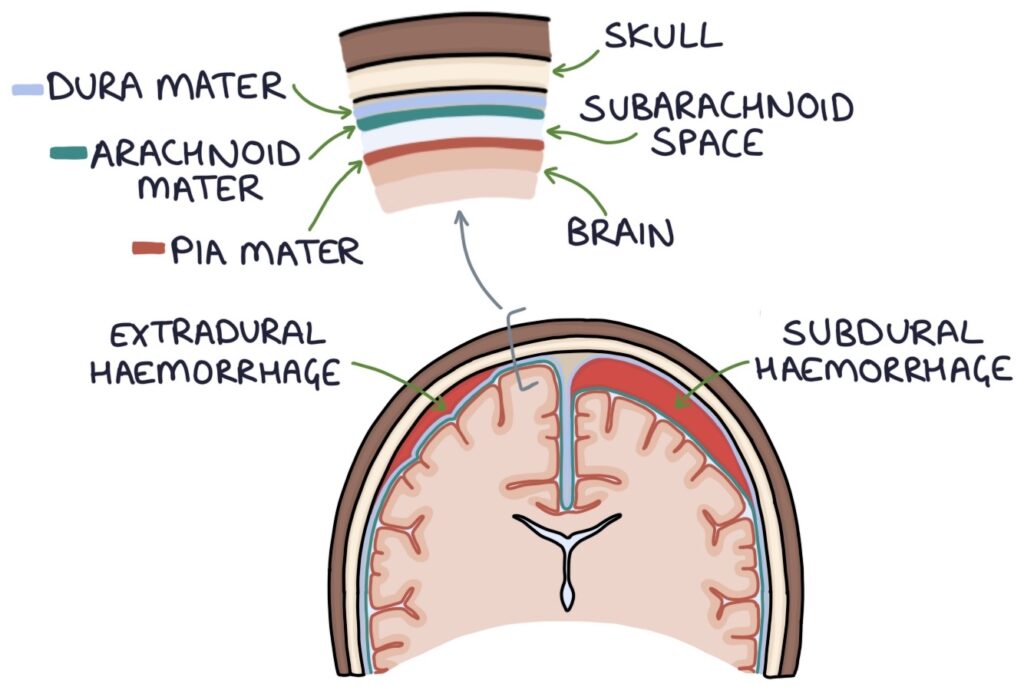
Intracranial haemorrhage refers to bleeding within the skull. There are four types:
- Extradural haemorrhage (bleeding between the skull and dura mater)
- Subdural haemorrhage (bleeding between the dura mater and arachnoid mater)
- Intracerebral haemorrhage (bleeding into brain tissue)
- Subarachnoid haemorrhage (bleeding in the subarachnoid space)
Intracerebral haemorrhage and subarachnoid haemorrhage account for 10-20% of strokes.
Risk Factors
- Head injuries
- Hypertension
- Aneurysms
- Ischaemic strokes (progressing to bleeding)
- Brain tumours
- Thrombocytopenia (low platelets)
- Bleeding disorders (e.g., haemophilia)
- Anticoagulants (e.g., DOACs or warfarin)
Presentation
Sudden-onset headache is a key feature. They can also present with:
- Seizures
- Vomiting
- Reduced consciousness
- Focal neurological symptoms (e.g., weakness)
Glasgow Coma Scale
The Glasgow Coma Scale (GCS) is a universal assessment tool for the level of consciousness. It is scored based on eyes, verbal response and motor response. The maximum score is 15/15, and the minimum is 3/15. A score of 8/15 needs airway support, as there is a risk of airway obstruction or aspiration, leading to hypoxia and brain injury.
|
Score |
Eyes |
Verbal Response |
Motor Response |
|
6 |
– |
– |
Obeys commands |
|
5 |
– |
Oriented |
Localises pain |
|
4 |
Spontaneous |
Confused |
Normal flexion |
|
3 |
Speech |
Inappropriate words |
Abnormal flexion |
|
2 |
Pain |
Incomprehensible sounds |
Extends |
|
1 |
None |
None |
None |
Extradural Haemorrhage
Extradural haemorrhage occurs between the skull and dura mater and is usually caused by a rupture of the middle meningeal artery in the temporoparietal region. It can be associated with a fracture of the temporal bone. On a CT scan, they have a bi-convex shape and are limited by the cranial sutures (they do not cross the sutures, which are the points where the skull bones join together).
A typical history is a young patient with a traumatic head injury and an ongoing headache. They have a period of improved neurological symptoms and consciousness, followed by a rapid decline over hours as the haematoma gets large enough to compress the intracranial contents.
Subdural Haemorrhage
Subdural haemorrhage occurs between the dura mater and arachnoid mater and is caused by a rupture of the bridging veins in the outermost meningeal layer. On a CT scan, they have a crescent shape and are not limited by the cranial sutures (they can cross over the sutures).
Subdural haemorrhages may occur in elderly and alcoholic patients, who have more atrophy in their brains, making the vessels more prone to rupture.
Intracerebral Haemorrhage
Intracerebral haemorrhage involves bleeding in the brain tissue. It presents similarly to an ischaemic stroke with sudden-onset focal neurological symptoms, such as limb or facial weakness, dysphasia or vision loss.
They can occur spontaneously or secondary to ischaemic stroke, tumours or aneurysm rupture.
They can occur anywhere in the brain tissue:
- Lobar intracerebral haemorrhage
- Deep intracerebral haemorrhage
- Intraventricular haemorrhage
- Basal ganglia haemorrhage
- Cerebellar haemorrhage
Subarachnoid Haemorrhage
Subarachnoid haemorrhage involves bleeding in the subarachnoid space, where the cerebrospinal fluid is located, between the pia mater and the arachnoid membrane. This is usually the result of a ruptured cerebral aneurysm.
The typical history is a sudden-onset occipital headache during strenuous activity, such as heavy lifting or sex. The sudden and severe onset leads to the “thunderclap headache” description.
Principles of Management
Immediate imaging (e.g., CT head) is required to establish the diagnosis. Bloods should include a full blood count (for platelets) and a coagulation screen.
Initial management will involve:
- Admission to a specialist stroke centre
- Discuss with a specialist neurosurgical centre to consider surgical treatment
- Consider intubation, ventilation and intensive care if they have reduced consciousness
- Correct any clotting abnormality (e.g., platelet transfusions or vitamin K for warfarin)
- Correct severe hypertension but avoid hypotension
Smaller bleeds may be managed conservatively with close monitoring and repeat imaging.
Surgical options for treating an extradural or subdural haematoma are:
- Craniotomy (open surgery by removing a section of the skull)
- Burr holes (small holes drilled in the skull to drain the blood)
Last updated September 2023
