Huntington’s disease (also called Huntington’s chorea) is an autosomal dominant genetic condition that causes progressive neurological dysfunction. It is a trinucleotide repeat disorder involving a genetic mutation in the HTT gene on chromosome 4, which codes for the huntingtin (HTT) protein.
Symptoms typically begin aged 30-50.
Trinucleotide Repeat Disorders
Nucleotides are the building blocks of DNA (adenine, cytosine, guanine and thymine). Trinucleotide repeats refer to repetitions of a sequence of three nucleotides (e.g., CAGCAGCAGCAGCAG).
Other examples of trinucleotide repeat disorders include:
- Fragile X syndrome
- Spinocerebellar ataxia
- Myotonic dystrophy
- Friedrich ataxia
Anticipation
Huntington’s chorea displays something called genetic anticipation. Anticipation is a feature of trinucleotide repeat disorders, where successive generations have more repeats in the gene, resulting in:
- Earlier age of onset
- Increased severity of disease
TOM TIP: Anticipation is a common concept tested in exams and worth remembering with Huntington’s.
Presentation
Huntington’s chorea presents with an insidious, progressive worsening of symptoms. It typically begins with cognitive, psychiatric or mood problems, followed by the development of movement disorders:
- Chorea (involuntary, random, irregular and abnormal body movements)
- Dystonia (abnormal muscle tone, leading to abnormal postures)
- Rigidity (increased resistance to the passive movement of a joint)
- Eye movement disorders
- Dysarthria (speech difficulties)
- Dysphagia (swallowing difficulties)
Management
Diagnosis is made by genetic testing via a specialist genetic centre and involves pre and post-test counselling.
There are currently no treatment options for slowing or stopping the progression of the disease.
Management of the condition involves supporting the person and their family:
- Breaking bad news effectively and supportively
- Genetic counselling regarding relatives, pregnancy and children
- Multidisciplinary team (MDT) input to support and maintain their quality of life
- Physiotherapy to improve mobility, maintain joint function and prevent contractures
- Speech and language therapy where there are speech and swallowing difficulties
- Tetrabenazine may be used for chorea symptoms
- Antidepressants (e.g., SSRIs) for depression
- Advanced directives to document their wishes as the disease progresses
- End-of-life care
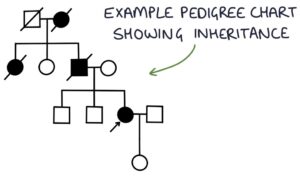
TOM TIP: An exam scenario may have you counsel someone about getting a genetic test for Huntington’s. The child of someone with the disease has a 50% chance of inheriting the faulty gene (it is autosomal dominant). They need to be 18 before they can decide whether to get tested. Your job is to provide information for the patient to make an informed decision for themselves, not to advise them whether to have a test or not. The outcome is usually that the patient will think about it further and return if they have further questions.
Prognosis
Huntington’s chorea is a progressive condition. Life expectance is around 10-20 years after the onset of symptoms. As the disease progresses, patients become more frail and susceptible to illness (e.g., infections, weight loss, falls and pressure ulcers). Death is often due to aspiration pneumonia. Suicide is also a common cause of death.
Last updated October 2023
Now, head over to members.zerotofinals.com and test your knowledge of this content. Testing yourself helps identify what you missed and strengthens your understanding and retention.

