Headaches are a very common presentation with a large number of causes. Causes include:
- Tension headaches
- Migraines
- Cluster headaches
- Secondary headaches
- Sinusitis
- Giant cell arteritis
- Glaucoma
- Intracranial haemorrhage
- Venous sinus thrombosis
- Subarachnoid haemorrhage
- Medication overuse
- Hormonal headache
- Cervical spondylosis
- Carbon monoxide poisoning
- Trigeminal neuralgia
- Raised intracranial pressure
- Brain tumours
- Meningitis
- Encephalitis
- Brain abscess
- Pre-eclampsia
Red Flags
Key red flags associated with a headache, indicating a possible serious underly cause, include:
- Fever, photophobia or neck stiffness (meningitis, encephalitis or brain abscess)
- New neurological symptoms (haemorrhage or tumours)
- Visual disturbance (giant cell arteritis, glaucoma or tumours)
- Sudden-onset occipital headache (subarachnoid haemorrhage)
- Worse on coughing or straining (raised intracranial pressure)
- Postural, worse on standing, lying or bending over (raised intracranial pressure)
- Vomiting (raised intracranial pressure or carbon monoxide poisoning)
- History of trauma (intracranial haemorrhage)
- History of cancer (brain metastasis)
- Pregnancy (pre-eclampsia)
Fundoscopy for papilloedema is an important. Papilloedema suggests raised intracranial pressure, which may be due to a brain tumour, benign intracranial hypertension or an intracranial bleed.
TOM TIP: Asking specifically about red flags demonstrates that you are thinking about serious causes. This will score extra points in OSCEs and help you document well when seeing patients.
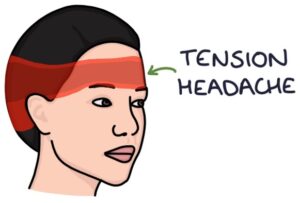
Tension Headaches
Tension headaches are very common. They typically cause a mild ache or pressure in a band-like pattern around the head. They develop and resolve gradually and do not produce visual changes.
Tension headaches may be associated with:
- Stress
- Depression
- Alcohol
- Skipping meals
- Dehydration
Management is with:
- Reassurance
- Simple analgesia (e.g., ibuprofen or paracetamol)
Amitriptyline is generally first-line for chronic or frequent tension headaches.
Secondary Headaches
Secondary headaches give a similar presentation to a tension headache but with a clear cause, such as:
- Infections (e.g., viral upper respiratory tract infection)
- Obstructive sleep apnoea
- Pre-eclampsia
- Head injury
- Carbon monoxide poisoning
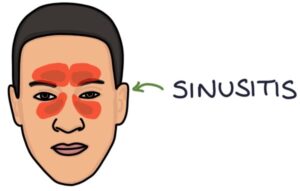
Sinusitis
Sinusitis refers to inflammation of the paranasal sinuses in the face. It typically causes pain and pressure following a recent viral upper respiratory tract infection. There may be tenderness and swelling on palpation of the affected areas. Most cases are caused by a viral infection and resolve within 2-3 weeks. Prolonged cases (over 10 days) may be treated with a steroid nasal spray or antibiotics (phenoxymethylpenicillin first-line).
Medication-Overuse Headache
Medication-overuse headache (also called analgesic headache) is a headache caused by frequent analgesia use. It gives similar non-specific features to a tension headache. Withdrawal of the analgesia is important in treating the headache, although this can be challenging in patients with long-term pain.
Hormonal Headache
Hormonal headaches are related to low oestrogen. They have similar features to migraines, with a unilateral, pulsatile headache associated with nausea. They are sometimes called menstrual migraines. They may occur:
- Two days before and the first three days of the menstrual period
- In the perimenopausal period
- Early pregnancy (headaches in the second half of pregnancy should prompt investigations for pre-eclampsia)
Triptans and NSAIDs (e.g., mefenamic acid) are treatment options.
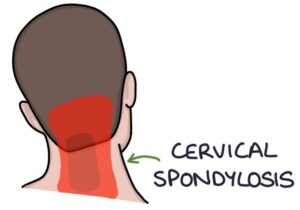
Cervical Spondylosis
Cervical spondylosis is a common condition caused by degenerative changes in the cervical spine. It causes neck pain, usually made worse by movement. It often presents with headaches.
Trigeminal Neuralgia
Trigeminal neuralgia causes intense facial pain in the distribution of the trigeminal nerve, which has three branches:
- Ophthalmic (V1)
- Maxillary (V2)
- Mandibular (V3)
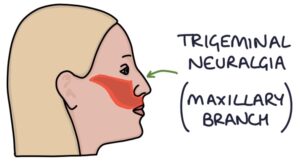
Trigeminal neuralgia can affect any combination of the branches. Over 90% of cases are unilateral. It is more common in patients with multiple sclerosis.
The pain comes on suddenly and can last seconds to hours. It may be described as an electricity-like, shooting, stabbing or burning pain. It may be triggered by touch, taking, eating, shaving or cold. Attacks may worsen over time.
NICE CKS (updated 2022) recommend carbamazepine as first-line for trigeminal neuralgia. Various surgical interventions are possible where the symptoms persist.
Last updated October 2023
Now, head over to members.zerotofinals.com and test your knowledge of this content. Testing yourself helps identify what you missed and strengthens your understanding and retention.

