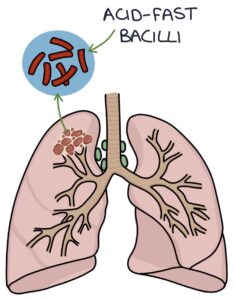
Tuberculosis (TB) is an infectious disease caused by Mycobacterium tuberculosis, a small rod-shaped bacteria (a bacillus). M. tuberculosis bacteria are very slow dividing and have high oxygen requirements, making them difficult to culture in a lab.
M. tuberculosis has a waxy coating that makes gram staining ineffective. They are resistant to the acids used in the staining procedure, described as “acid-fast”, making them acid-fast bacilli. Special staining is required, using the Zeihl-Neelsen stain, which turns them bright red against a blue background.
TOM TIP: A common exam question involves a patient with a chronic cough and night sweats. Sputum culture grows “acid-fast bacilli” that stain red with “Zeihl-Neelsen staining”. These keywords are worth remembering.
Multidrug-resistant TB (MDR-TB) are strains that are resistant to more than one TB drug (e.g., isoniazid and rifampicin), making them difficult to treat.
Disease Course
Tuberculosis is mostly spread by inhaling saliva droplets from infected people. Once in the body, there are several possible outcomes:
- Immediate clearance of the bacteria (in most cases)
- Primary active tuberculosis (active infection after exposure)
- Latent tuberculosis (presence of the bacteria without being symptomatic or contagious)
- Secondary tuberculosis (reactivation of latent tuberculosis to active infection)
When the immune system cannot control the infection, disseminated and severe disease can develop, referred to as miliary tuberculosis.
Latent tuberculosis is present when the immune system encapsulates the bacteria and stops the progression of the disease. Patients with latent tuberculosis have no symptoms and cannot spread the bacteria. Most otherwise healthy patients with latent tuberculosis never develop an active infection. When latent tuberculosis reactivates, and an infection develops, usually due to immunosuppression, this is called secondary tuberculosis.
The most common site for TB infection is in the lungs, where it gets plenty of oxygen. Extrapulmonary tuberculosis refers to disease in other areas:
- Lymph nodes
- Pleura
- Central nervous system
- Pericardium
- Gastrointestinal system
- Genitourinary system
- Bones and joints
- Skin (cutaneous tuberculosis)
A cold abscess describes a firm, painless abscess caused by tuberculosis, usually in the neck. They do not have the inflammation, redness and pain you expect from an acutely infected abscess.
Risk Factors
- Close contact with active tuberculosis (e.g., a household member)
- Immigrants from areas with high tuberculosis prevalence
- People with relatives or close contacts from countries with a high rate of TB
- Immunocompromised (e.g., HIV or immunosuppressant medications)
- Malnutrition, homelessness, drug users, smokers and alcoholics
BCG Vaccine
The Bacillus Calmette–Guérin (BCG) vaccine involves an intradermal injection of live attenuated (weakened) Mycobacterium bovis bacteria (a close relative of M. tuberculosis that does not cause disease in humans). This creates an immune response, providing lasting immunity against M. tuberculosis without causing infection. The vaccine protects against severe and complicated TB but less against pulmonary TB.
Before vaccination, patients are tested with the Mantoux test and only given the vaccine if this test is negative. They are also assessed for the possibility of immunosuppression and HIV due to the risks related to a live vaccine.
The BCG vaccine is not part of the routine vaccination schedule. It is offered to patients at increased risk of TB, such as those from areas of high TB prevalence, with close contact with TB (e.g., family members) and healthcare workers.
Presentation
Tuberculosis typically presents with chronic, gradually worsening symptoms. Most cases involve pulmonary disease, often with systemic symptoms.
Typical signs and symptoms of tuberculosis include:
- Cough
- Haemoptysis (coughing up blood)
- Lethargy
- Fever or night sweats
- Weight loss
- Lymphadenopathy
- Erythema nodosum (tender, red nodules on the shins caused by inflammation of the subcutaneous fat)
- Spinal pain in spinal tuberculosis (also known as Pott’s disease of the spine)
Investigations
Tuberculosis can be challenging to diagnose. The bacteria grow very slowly in a culture, cannot be stained with traditional gram stains and require specialist stains (e.g., Ziehl-Neelsen stain).
There are two tests for an immune response to tuberculosis caused by previous infection, latent TB or active TB:
- Mantoux test
- Interferon‑gamma release assay (IGRA)
In patients where active disease is suspected, investigations to support the diagnosis include:
- Chest x-ray
- Cultures
Mantoux Test
The Mantoux test involves injecting tuberculin into the intradermal space on the forearm. Tuberculin is a collection of tuberculosis proteins isolated from the bacteria. It does not contain any live bacteria.
The infection creates a bleb under the skin. After 72 hours, the test is “read”. This involves measuring the induration of the skin at the injection site. An induration of 5mm or more is considered a positive result.
Interferon-Gamma Release Assays
IGRA involves mixing a blood sample with antigens from the M. tuberculosis bacteria. After previous contact with M. tuberculosis, white blood cells become sensitised to the bacteria antigens and will release interferon-gamma on further contact. A positive result is when interferon-gamma is released during the test.
Chest X-ray
Primary tuberculosis may show patchy consolidation, pleural effusions and hilar lymphadenopathy.
Reactivated tuberculosis may show patchy or nodular consolidation with cavitation (gas-filled spaces), typically in the upper zones.
Disseminated miliary tuberculosis gives an appearance of millet seeds uniformly distributed across the lung fields.
TOM TIP: Disseminated miliary tuberculosis gives a characteristic appearance of “millet seeds” on a chest x-ray, with many small (1-3mm) nodules disseminated throughout the lung fields. This makes it a popular spot diagnosis in exams. It is worth becoming familiar with the appearance.
Cultures
Culture samples are ideally collected before starting treatment. This allows testing for drug resistance. However, cultures can take several months. Treatment is usually started while waiting for the culture results.
There are several ways to collect cultures:
- Sputum cultures (3 separate sputum samples are collected)
- Mycobacterium blood cultures (require special blood culture bottle)
- Lymph node aspiration or biopsy
The NICE guidelines on tuberculosis (2016) describe “deep cough” sputum samples. If they are not producing enough sputum, the options are:
- Sputum induction with nebulised hypertonic saline
- Bronchoscopy and bronchoalveolar lavage (saline is used to wash the airways and collect a sample)
Nucleic Acid Amplification Tests
Nucleic acid amplification tests (NAAT) assess for the genetic material of a pathogen. To detect tuberculosis DNA, NAAT is performed on a sample containing the bacteria (e.g., a sputum sample). It provides information about the bacteria faster than traditional culture, including drug resistance. NAAT is used for:
- Diagnosing tuberculosis in patients with HIV or aged under 16
- Risk factors for multidrug resistance (where the results would alter management)
Treatment
Latent tuberculosis is treated with either:
- Isoniazid and rifampicin for 3 months
- Isoniazid for 6 months
The treatment for active tuberculosis can be remembered with the RIPE mnemonic:
- R – Rifampicin for 6 months
- I – Isoniazid for 6 months
- P – Pyrazinamide for 2 months
- E – Ethambutol for 2 months
TOM TIP: Remember that isoniazid causes peripheral neuropathy, and pyridoxine (vitamin B6) is co-prescribed to help prevent this. An exam question might say, “…are started on R, I, P and E. What else should be prescribed?” The answer would be pyridoxine or vitamin B6.
Other management options to consider include:
- Testing for other infectious diseases (e.g., HIV, hepatitis B and hepatitis C)
- Testing contacts for tuberculosis
- Notifying UK Health Security Agency (UKHSA) of suspected cases
- Isolating patients with active tuberculosis to prevent spread (usually for at least 2 weeks of treatment)
- A specialist MDT guides management and follow-up
- Individualised regimes are required for multidrug‑resistant tuberculosis and extrapulmonary disease
In hospitals, negative pressure rooms are used to prevent airborne spread. Negative pressure rooms have ventilation systems that actively remove air to prevent it from spreading onto the ward.
Side Effects of Treatment
Rifampicin can cause red/orange discolouration of secretions, such as urine and tears. It is a potent inducer of the cytochrome P450 enzymes and reduces the effects of drugs metabolised by this system, such as the combined contraceptive pill.
Isoniazid can cause peripheral neuropathy. Pyridoxine (vitamin B6) is co-prescribed to reduce the risk.
Pyrazinamide can cause hyperuricaemia (high uric acid levels), resulting in gout and kidney stones.
Ethambutol can cause colour blindness and reduced visual acuity.
Rifampicin, isoniazid and pyrazinamide are all associated with hepatotoxicity.
TOM TIP: A common exam question asks “…has recently started treatment for tuberculosis. They notice _____. Which medication is most likely to be implicated?” Numbness or unusual sensations in their feet implicates isoniazide (“I’m-so-numb-azid”). Difficulty recognising colours implicates ethambutol (“eye-thambutol”). Urine or tears that are orange or red implicates rifampicin (“red-I’m-pissin’”).
Last updated August 2023
