Septic arthritis refers to an infection in a joint.
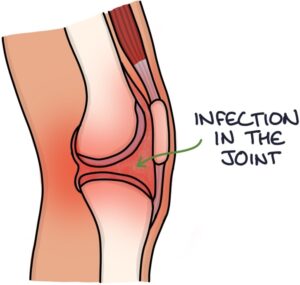
Infection in a joint is a medical emergency. The infection can rapidly destroy the joint and cause systemic illness. Septic arthritis has a mortality of around 10%.
Infection may occur in a native joint (an original joint) or a prosthetic joint replacement.
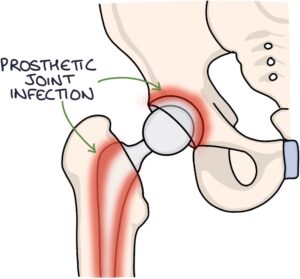
Infection in a prosthetic joint is a big problem and happens in around 1% of joint replacements. Extensive measures are taken to prevent it, such as perioperative prophylactic antibiotics. It is more likely to occur in revision surgery than in the initial joint replacement.
Presentation
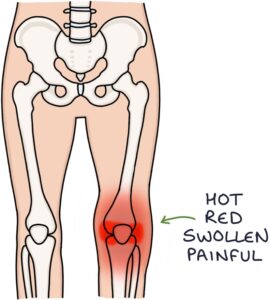
Septic arthritis usually only affects a single joint, often a knee. It presents with a rapid onset of:
- A hot, red, swollen and painful joint
- Stiffness and reduced range of motion
- Systemic symptoms, such as fever, lethargy and sepsis
Common Bacteria
Staphylococcus aureus is the most common causative organism.
Other bacteria:
- Neisseria gonorrhoea (gonococcus) in sexually active individuals
- Group A Streptococcus (most commonly Streptococcus pyogenes)
- Haemophilus influenzae
- Escherichia coli (E. coli)
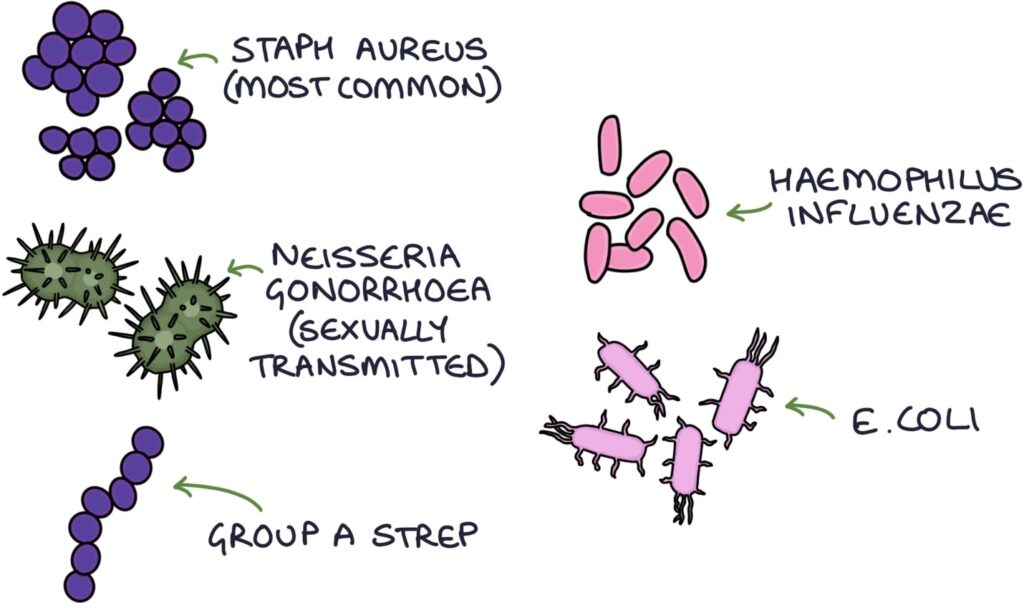
TOM TIP: In a young patient presenting with a single acutely swollen joint, consider gonococcal septic arthritis until proven otherwise. The gram stain reveals a gram-negative diplococcus. Urinary or genital symptoms should also make you think of reactive arthritis (once gonococcal septic arthritis is excluded).
Differential Diagnosis
The key differential diagnoses of a single warm swollen joint are:
- Gout (joint fluid shows urate crystals that are negatively birefringent of polarised light)
- Pseudogout (joint fluid shows rod-shaped calcium pyrophosphate crystals that are positively birefringent)
- Reactive arthritis (typically triggered by urethritis or gastroenteritis and associated with conjunctivitis)
- Haemarthrosis (bleeding into the joint, usually after trauma)
Management
Have a low threshold for suspecting septic arthritis, particularly in immunosuppressed patients. Delayed treatment has significant consequences. Joint fluid examination is usually required to exclude septic arthritis.
There will be a local acute hot joint policy to guide what team admits the patient (e.g., orthopaedics, rheumatology or infectious diseases), what antibiotics to use and for how long.
Joint aspiration is performed before starting antibiotics. The sample is sent for gram staining, crystal microscopy, culture and antibiotic sensitivities. The joint fluid may be purulent (full of pus). The gram stain result is usually available quickly and may give a clue about the organism. Culture and antibiotic sensitivities take longer.

Empirical IV antibiotics should be given until the sensitivities are known.
Antibiotics are usually continued for 4-6 weeks in total (initially IV, then oral). The choice of antibiotic depends on local guidelines. Example choices are:
- Flucloxacillin (often first-line)
- Clindamycin (penicillin allergy)
- Vancomycin (if MRSA is suspected)
Ceftriaxone is typically used for treating Neisseria gonorrhoea.
Last updated July 2023
Now, head over to members.zerotofinals.com and test your knowledge of this content. Testing yourself helps identify what you missed and strengthens your understanding and retention.