Being infected with the human immunodeficiency virus (HIV) is referred to as being HIV positive.
Acquired immunodeficiency syndrome (AIDS) occurs when HIV is not treated, the disease progresses, and the person becomes immunocompromised. Immunodeficiency leads to opportunistic infections and AIDS-defining illnesses.
Basics
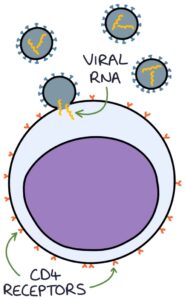
HIV is an RNA retrovirus. HIV-1 is the most common type. HIV-2 is mainly found in West Africa. The virus enters and destroys the CD4 T-helper cells of the immune system.
An initial seroconversion flu-like illness occurs within a few weeks of infection. The infection is then asymptomatic until the condition progresses to immunodeficiency. Disease progression may occur years after the initial infection.
Transmission
HIV is not transmitted through day-to-day activities, including kissing. It is spread through:
- Unprotected anal, vaginal or oral sexual activity
- Mother to child at any stage of pregnancy, birth or breastfeeding (called vertical transmission)
- Mucous membrane, blood or open wound exposure to infected blood or bodily fluids (e.g., sharing needles, needle-stick injuries or blood splashed in an eye)
AIDS-Defining Illnesses
There is a long list of AIDS-defining illnesses associated with end-stage HIV infection. These occur where the CD4 count has dropped to a level that allows for unusual opportunistic infections and malignancies to appear.
Examples of AIDS-defining illnesses include:
- Kaposi’s sarcoma
- Pneumocystis jirovecii pneumonia (PCP)
- Cytomegalovirus infection
- Candidiasis (oesophageal or bronchial)
- Lymphomas
- Tuberculosis
Screening
Many people with HIV do not know they are infected, and these patients are at risk of complications and spreading the disease. Generally, the earlier a patient is diagnosed, the better the outcome. HIV is a treatable condition, and most patients are fit and healthy on treatment. There should be a low threshold for HIV testing. Patients with any risk factors should be tested. All patients accessing sexual health, antenatal and substance misuse services are offered testing.
Verbal consent should be documented before a test. However, BHIVA (2023) have draft guidelines for assumed consent (unless the patient voluntarily chooses to opt-out) to HIV screening on blood tests taken in emergency departments (provided posters and leaflets are available).
The fourth-generation laboratory test for HIV checks for antibodies to HIV and the p24 antigen. It has a window period of 45 days, meaning it can take up to 45 days after exposure to the virus for the test to turn positive. A negative result within 45 days of exposure is unreliable. More than 45 days after exposure, a negative result is reliable.
Point-of-care tests for HIV antibodies give a result within minutes. They have a 90-day window period.
Patients at risk of HIV can request home testing kits, either:
- Self-sampling kits to be posted to the lab (fourth-generation tests for antibodies and the p24 antigen)
- Point-of-care tests (antibodies only)
Monitoring
Testing the CD4 count gives the number of CD4 cells in the blood. These are the cells destroyed by the virus. The lower the count, the higher the risk of opportunistic infection:
- 500-1200 cells/mm3 is the normal range
- Under 200 cells/mm3 puts the patient at high risk of opportunistic infections
Testing for HIV RNA per ml of blood indicates the viral load. An undetectable viral load means the level is below the recordable range (usually 20 copies/ml). The viral load can be in the hundreds of thousands in untreated HIV.
Treatment
Specialist HIV, infectious disease or GUM centres manage patients with HIV.
Treatment involves a combination of antiretroviral therapy (ART) medications. ART is offered to everyone diagnosed with HIV, irrespective of viral load or CD4 count. Some regimes involve only a single combination tablet, taken once daily, with the potential to suppress the infection completely. Genotypic resistance testing can establish the resistance of each HIV strain to different medications to help guide treatment.
There are several classes of antiretroviral therapy medications:
- Protease inhibitors (PI)
- Integrase inhibitors (II)
- Nucleoside reverse transcriptase inhibitors (NRTI)
- Non-nucleoside reverse transcriptase inhibitors (NNRTI)
- Entry inhibitors (EI)
The usual starting regime is two NRTIs (e.g., tenofovir plus emtricitabine) plus a third agent (e.g., bictegravir).
Treatment aims to achieve a normal CD4 count and undetectable viral load. Generally, when a patient has a normal CD4 and an undetectable viral load on ART, physical health problems (e.g., routine chest infections) are treated the same as those without HIV.
TOM TIP: When prescribing for patients on ART, be aware and carefully check for any medication interactions (hiv-druginteractions.org is a helpful website).
Additional Management
Prophylactic co-trimoxazole is given to all HIV positive patients with a CD4 count under 200/mm3 to protect against pneumocystis jirovecii pneumonia (PCP).
HIV infection increases the risk of developing cardiovascular disease. Patients with HIV have close monitoring of cardiovascular risk factors, such as blood lipids. Interventions to reduce the risk (e.g., statins) may be recommended.
Yearly cervical smears are recommended in HIV as it increases the risk of human papillomavirus (HPV) infection and cervical cancer.
Vaccinations should be up to date, including against influenza (yearly), pneumococcal, HPV and hepatitis A and B. Live vaccines (e.g., BCG and typhoid) are avoided.
Reproductive Health
Correct use of condoms protects against spreading HIV. Effective treatment combined with an undetectable viral load appears to prevent the spread of HIV, even during unprotected sex (although there is still a risk of other STIs).
Preventing Transmission During Birth
This information here is an oversimplified illustration of the BHIVA guidelines.
The mother’s viral load will determine the mode of delivery:
|
Viral Load |
Delivery |
|
Under 50 copies/ml |
Normal vaginal delivery |
|
Over 50 copies/ml |
Consider a pre-labour caesarean section |
|
Over 400 copies/ml |
Pre-labour caesarean section is recommended |
IV zidovudine is given as an infusion during labour and delivery if the viral load is unknown or above 1000 copies/ml.
Prophylaxis may be given to the baby, depending on the mother’s viral load:
- Low-risk babies (mother’s viral load is under 50 copies per ml) are given zidovudine for 2-4 weeks
- High-risk babies are given zidovudine, lamivudine and nevirapine for four weeks
Breast Feeding
HIV can be transmitted during breastfeeding. The risk is reduced if the mother’s viral load is undetectable but not eliminated. Therefore, the safest option is to avoid breastfeeding. However, if the mother is adamant and the viral load is undetectable, sometimes it is attempted with close monitoring by the HIV team.
Prophylaxis
Post-exposure prophylaxis (PEP) can be used after exposure to reduce the risk of transmission. PEP is not 100% effective and must be commenced within a short window of opportunity (less than 72 hours). The sooner it is started, the better. A risk assessment of the probability of developing HIV should be balanced against the side effects of PEP.
PEP involves a combination of ART therapy. The current regime is emtricitabine/tenofovir (Truvada) and raltegravir for 28 days.
Pre-exposure prophylaxis (PrEP) is also available to take before exposure to reduce the risk of transmission. The usual choice is emtricitabine/tenofovir (Truvada).
Last updated August 2023
