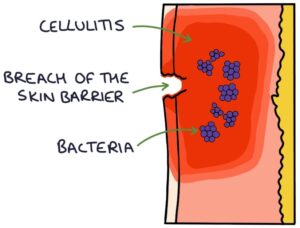
Cellulitis is an infection of the skin and the soft tissues underneath. The skin forms a physical barrier between the environment and soft tissues. When a patient presents with cellulitis, look for a breach in the skin barrier and a point of entry for the bacteria. This may be due to skin trauma, eczema, fungal nail infections or ulcers.
Presentation
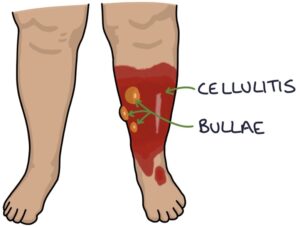
Skin changes in cellulitis include:
- Erythema (red discolouration)
- Warm or hot to touch
- Tense
- Thickened
- Oedematous
- Bullae (fluid-filled blisters)
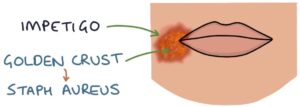
- A golden-yellow crust indicates a Staphylococcus aureus infection
Patients may be systemically unwell, including having sepsis.
Causes
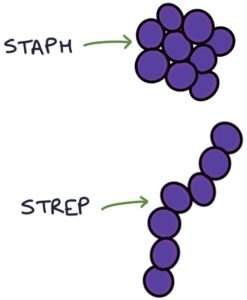
The most common causes are:
- Staphylococcus aureus
- Group A streptococcus (mainly streptococcus pyogenes)
- Group C streptococcus (mainly streptococcus dysgalactiae)
MRSA should be considered, particularly in patients the repeated hospital admissions and antibiotics.
Eron Classification
The Eron classification assesses the severity of cellulitis:
- Class 1 – no systemic toxicity or comorbidity
- Class 2 – systemic toxicity or comorbidity
- Class 3 – significant systemic toxicity or significant comorbidity
- Class 4 – sepsis or life-threatening infection
Management
Class 3 and 4 cellulitis requires admission for intravenous antibiotics. Admission is also considered for frail, very young or immunocompromised patients and those with facial, periorbital or orbital cellulitis.
Flucloxacillin is the usual first-line antibiotic for cellulitis, either oral or intravenous. It is particularly effective against Staphylococcus aureus and also works well against other gram-positive cocci.
Alternatives:
- Clarithromycin
- Clindamycin
- Co-amoxiclav (the usual first choice for cellulitis near the eyes or nose)
Last updated July 2023
Now, head over to members.zerotofinals.com and test your knowledge of this content. Testing yourself helps identify what you missed and strengthens your understanding and retention.

