Thrombocytopenia describes a low platelet count. The normal platelet count is 150-450 x 109/L. There is a long list of causes of a low platelet count. They can be split into problems with production or destruction.
Reduced platelet production can occur with:
- Certain viral infections (e.g., Epstein-Barr virus, cytomegalovirus and HIV)
- B12 deficiency
- Folic acid deficiency
- Liver failure, causing reduced thrombopoietin production by the liver
- Leukaemia
- Myelodysplastic syndrome
- Chemotherapy
Increased platelet destruction can occur with:
- Medications (e.g., sodium valproate and methotrexate)
- Alcohol
- Immune thrombocytopenic purpura (ITP)
- Thrombotic thrombocytopenic purpura (TTP)
- Heparin-induced thrombocytopenia (HIT)
- Haemolytic uraemic syndrome (HUS)
Presentation
Mild thrombocytopenia may be asymptomatic and found incidentally on a full blood count.
Platelet counts below 50 x 109/L will result in easy bruising and prolonged bleeding times. It may present with:
- Nosebleeds
- Bleeding gums
- Heavy periods
- Easy bruising
- Haematuria (blood in the urine)
- Rectal bleeding
Platelet counts below 10 x 109/L are at high risk for spontaneous bleeding. Particularly concerning are:
- Intracranial haemorrhage
- Gastrointestinal bleeding
Differential Diagnosis of Abnormal Bleeding
The clotting system creates blood clots to stop bleeding. There are several ways this system can malfunction. The top differentials of abnormal or prolonged bleeding to remember are:
- Thrombocytopenia
- Von Willebrand disease
- Haemophilia A and haemophilia B
- Disseminated intravascular coagulation (usually secondary to sepsis)
Immune Thrombocytopenic Purpura
Immune thrombocytopenic purpura (ITP) can also be called autoimmune thrombocytopenic purpura, idiopathic thrombocytopenic purpura and primary thrombocytopenic purpura. They all refer to the same condition.
ITP is a condition where antibodies are created against platelets. An immune response against platelets leads to their destruction and a low platelet count (thrombocytopenia).

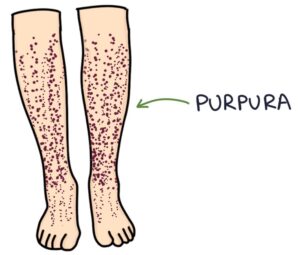
It characteristically presents with purpura, which are non-blanching lesions caused by bleeding under the skin.
Care involves monitoring the platelet count, controlling blood pressure, and suppressing menstrual periods.
Management options include:
- Prednisolone (steroids)
- IV immunoglobulins
- Thrombopoietin receptor agonists (e.g., avatrombopag)
- Rituximab (a monoclonal antibody that targets B cells)
- Splenectomy
TOM TIP: B cells produce antibodies. Rituximab is worth remembering as a monoclonal antibody that targets the CD20 proteins on the surface of B cells. By attacking B cells and reducing their numbers, it reduces the production of the antibodies that are responsible for autoimmune disease. It treats many autoimmune conditions, from rheumatoid arthritis to ITP.
Thrombotic Thrombocytopenic Purpura
Thrombotic thrombocytopenic purpura (TTP) is a condition where tiny thrombi develop throughout the small vessels, using up platelets. As the problem is in the small vessels, it is described as a microangiopathy. It causes:
- Thrombocytopenia
- Purpura
- Tissue ischaemia and end-organ damage
Thrombi develop due to a problem with a specific protein called ADAMTS13. This protein normally:
- Inactivates von Willebrand factor
- Reduces platelet adhesion to vessel walls
- Reduces clot formation
Deficiency in the ADAMTS13 protein can be due to:
- An inherited genetic mutation (hereditary)
- Autoimmune disease, where antibodies are created against the protein (acquired)
Treatment is guided by a haematologist and may involve plasma exchange, steroids and rituximab.
Heparin-Induced Thrombocytopenia
Heparin-induced thrombocytopenia (HIT) involves the development of antibodies against platelets in response to heparin (usually unfractionated heparin, but it can occur with low-molecular-weight heparin). Heparin-induced antibodies target a protein on platelets called platelet factor 4 (PF4).
The condition typically presents around 5-10 days after starting treatment with heparin. HIT antibodies bind to platelets and activate the clotting system, causing a hypercoagulable state and thrombosis (e.g., deep vein thrombosis). They also break down platelets and cause thrombocytopenia. Therefore, there is a counterintuitive situation where a patient is on heparin, has a low platelet count, and develops abnormal blood clots.
Diagnosis is by testing for HIT antibodies on a blood sample. Management involves stopping heparin and using an alternative anticoagulant guided by a specialist (e.g., fondaparinux or argatroban).
Last updated August 2023
Now, head over to members.zerotofinals.com and test your knowledge of this content. Testing yourself helps identify what you missed and strengthens your understanding and retention.

