Blood is made of plasma (the liquid of the blood), which contains red blood cells, white blood cells, platelets and clotting factors, such as fibrinogen.
Once the clotting factors are removed from the blood, what is left is called the serum. Serum contains:
- Glucose
- Electrolytes, such as sodium and potassium
- Proteins, such as immunoglobulins (antibodies) and hormones
Blood Cells
Blood cells develop in the bone marrow. Bone marrow is mostly found in the pelvis, vertebrae, ribs and sternum. Familiarity with the different cell lines helps you understand conditions where things go wrong.
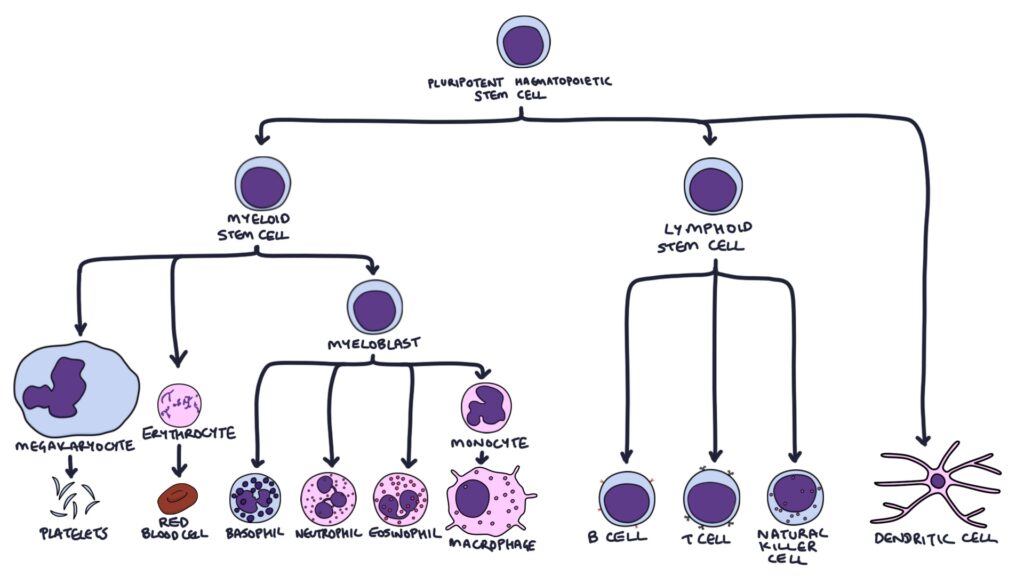
Pluripotent haematopoietic stem cells are undifferentiated cells that can transform into various blood cells. They initially become:
- Myeloid stem cells
- Lymphoid stem cells
- Dendritic cells (via different intermediate stages)
Red blood cells (RBC) develop from reticulocytes, which originate from myeloid stem cells. Reticulocytes are immature red blood cells. Red blood cells survive around four months (120 days).
Platelets are made by megakaryocytes, which develop from the myeloid stem cells. The lifespan of platelets is around ten days. The normal count is 150 – 450 x 109/L. Their role is to clump together (platelet aggregation) and plug gaps where blood clots need to form.
White Blood Cells
Myeloid stem cells become myeloblasts, which can become:
- Monocytes then macrophages
- Neutrophils
- Eosinophils
- Mast cells
- Basophils
Lymphocytes come from the lymphoid stem cells and become B cells or T cells.
B lymphocytes (B cells) mature in the bone marrow and differentiate into:
- Plasma cells
- Memory B cells
T lymphocytes (T cells) mature in the thymus gland and differentiate into:
- CD4 cells (T helper cells)
- CD8 cells (cytotoxic T cells)
- Natural killer cells
Blood Film Findings
A blood film involves the manual examination of the blood using a microscope, looking for abnormal shapes, sizes and inclusions (contents) of the cells. The key abnormal findings are summarised below.
Anisocytosis refers to a variation in the size of the red blood cells. These can be seen in myelodysplastic syndrome and many types of anaemia (e.g., iron deficiency, pernicious and autoimmune haemolytic anaemia).
Target cells are red blood cells with a central pigmented area surrounded by a pale area, surrounded by a ring of thicker cytoplasm on the outside. They look like a bull’s eye target. These are mostly seen in iron deficiency anaemia and post-splenectomy.
Heinz bodies are individual blobs (inclusions) seen inside red blood cells. These blobs are denatured (damaged) haemoglobin. They are mostly seen in G6PD deficiency and alpha-thalassaemia.
Howell-Jolly bodies are individual blobs of DNA material seen inside red blood cells. The spleen would Normally remove red blood cells with this DNA material inside. They are seen in patients after a splenectomy or with a non-functioning spleen (e.g., caused by sickle cell anaemia). They are also seen in severe anaemia, where the body is regenerating red blood cells very fast.
Reticulocytes are immature red blood cells. They are slightly larger than normal red blood cells (erythrocytes) and still have RNA material in them. The RNA has a reticular (“mesh-like”) appearance inside the cell. It is normal for about 1% of red blood cells to be reticulocytes. This percentage goes up where there is a rapid turnover of red blood cells, such as with haemolytic anaemia, where the bone marrow is actively trying to replace lost cells.
Schistocytes are fragments of red blood cells. They indicate that red blood cells are being physically damaged during their journey through the circulation. Microangiopathic haemolytic anaemia (MAHA) occurs when small blood clots (thrombi) obstruct small blood vessels. These obstructions churn the red blood cells, causing haemolysis (rupture). The key causes of MAHA are haemolytic uraemic syndrome (HUS), disseminated intravascular coagulation (DIC) and thrombotic thrombocytopenic purpura (TTP). Schistocytes can also be seen in metallic heart valve replacement as the metallic valves damage the red blood cells.
Sideroblasts are immature red blood cells with a nucleus surrounded by iron blobs. Sideroblastic anaemia occurs when the bone marrow cannot incorporate iron into the haemoglobin molecules. This is due to either a genetic defect or myelodysplastic syndrome.
Smudge cells are ruptured white blood cells that occur while preparing the blood film when the cells are aged or fragile. They are particularly associated with chronic lymphocytic leukaemia.
Spherocytes are sphere-shaped red blood cells without the bi-concave disk shape. They can indicate autoimmune haemolytic anaemia or hereditary spherocytosis.
Last updated August 2023
Now, head over to members.zerotofinals.com and test your knowledge of this content. Testing yourself helps identify what you missed and strengthens your understanding and retention.

