Anaemia is defined as a low concentration of haemoglobin in the blood. This is the consequence of an underlying disease, not a disease itself. An- means without, and -aemia refers to blood.
Haemoglobin is a protein found in red blood cells. Haemoglobin is responsible for picking up oxygen in the lungs and transporting it to the body’s cells. Iron is essential in creating haemoglobin and forms part of it’s structure.
The mean cell volume (MCV) refers to the size of the red blood cells and is highly relevant in anaemic patients. The normal ranges are:
|
Haemoglobin |
Mean Cell Volume (MCV) |
|
|
Women |
120 – 165 grams/litre |
80-100 femtolitres |
|
Men |
130 -180 grams/litre |
80-100 femtolitres |
Causes
Anaemia is divided into three categories based on the mean cell volume:
- Microcytic anaemia (low MCV)
- Normocytic anaemia (normal MCV)
- Macrocytic anaemia (large MCV)
The mnemonic for remembering the causes of microcytic anaemia is “TAILS”:
- T – Thalassaemia
- A – Anaemia of chronic disease
- I – Iron deficiency anaemia
- L – Lead poisoning
- S – Sideroblastic anaemia
Anaemia of chronic disease often occurs with chronic kidney disease due to reduced production of erythropoietin by the kidneys, the hormone responsible for stimulating red blood cell production. Treatment is with erythropoietin.
There are 3 As and 2 Hs for normocytic anaemia:
- A – Acute blood loss
- A – Anaemia of chronic disease
- A – Aplastic anaemia
- H – Haemolytic anaemia
- H – Hypothyroidism
Macrocytic anaemia can be megaloblastic or normoblastic. Megaloblastic anaemia results from impaired DNA synthesis, preventing the cells from dividing normally. Rather than dividing, they grow into large, abnormal cells.
Megaloblastic anaemia is caused by:
- B12 deficiency
- Folate deficiency
Normoblastic macrocytic anaemia is caused by:
- Alcohol
- Reticulocytosis (usually from haemolytic anaemia or blood loss)
- Hypothyroidism
- Liver disease
- Drugs, such as azathioprine
Reticulocytosis refers to an increased concentration of reticulocytes (immature red blood cells). This happens when there is a rapid turnover of red blood cells, such as with haemolytic anaemia or blood loss.
Symptoms
There are many generic symptoms of anaemia:
- Tiredness
- Shortness of breath
- Headaches
- Dizziness
- Palpitations
- Worsening of other conditions, such as angina, heart failure or peripheral arterial disease
Symptoms specific to iron deficiency anaemia include:
- Pica (dietary cravings for abnormal things, such as dirt or soil)
- Hair loss
Signs
Generic signs of anaemia include:
- Pale skin
- Conjunctival pallor
- Tachycardia
- Raised respiratory rate
Signs of specific causes of anaemia include:
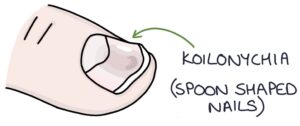
- Koilonychia refers to spoon-shaped nails and can indicate iron deficiency anaemia
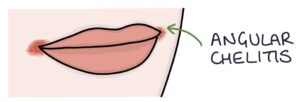
- Angular cheilitis can indicate iron deficiency anaemia
- Atrophic glossitis is a smooth tongue due to atrophy of the papillae and can indicate iron deficiency anaemia
- Brittle hair and nails can indicate iron deficiency anaemia
- Jaundice can indicate haemolytic anaemia
- Bone deformities can indicate thalassaemia
- Oedema, hypertension and excoriations on the skin can indicate chronic kidney disease
Investigations
Blood tests depend on the suspected cause. Possible blood tests include:
- Full blood count for haemoglobin and mean cell volume
- Reticulocyte count (indicates red blood cell production)
- Blood film for abnormal cells and inclusions
- Renal profile for chronic kidney disease
- Liver function tests for liver disease and bilirubin (raised in haemolysis)
- Ferritin (iron)
- B12 and folate
- Intrinsic factor antibodies for pernicious anaemia
- Thyroid function tests for hypothyroidism
- Coeliac disease serology (e.g., anti-tissue transglutaminase antibodies)
- Myeloma screening (e.g., serum protein electrophoresis)
- Haemoglobin electrophoresis for thalassaemia and sickle cell disease
- Direct Coombs test for autoimmune haemolytic anaemia
A colonoscopy and oesophagogastroduodenoscopy (OGD) are indicated for unexplained iron deficiency anaemia to exclude gastrointestinal cancer as a source of bleeding.
A bone marrow biopsy is indicated for unexplained anaemia or possible malignancy (e.g., leukaemia or myeloma).
Last updated August 2023
Now, head over to members.zerotofinals.com and test your knowledge of this content. Testing yourself helps identify what you missed and strengthens your understanding and retention.

