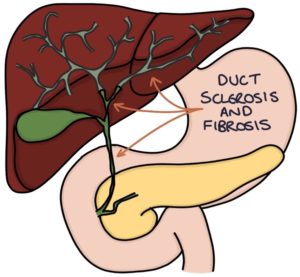
Primary sclerosing cholangitis is a condition where the intrahepatic and extrahepatic bile ducts become inflamed and damaged, developing strictures that obstruct the flow of bile out of the liver and into the intestines. Sclerosis refers to the stiffening and hardening of the bile ducts, and cholangitis is inflammation of the bile ducts. Chronic bile obstruction eventually leads to liver inflammation (hepatitis), fibrosis and cirrhosis.
The cause is unclear and thought to be combined genetic and environmental factors. There is a strong association with ulcerative colitis, with around 70% of cases occurring alongside pre-existing ulcerative colitis. Less commonly, it can be associated with Crohn’s disease.
The key risk factors for primary sclerosing cholangitis are:
- Male
- Aged 30-40
- Ulcerative colitis
- Family history
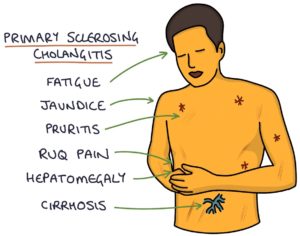
Presentation
Often patients are asymptomatic at diagnosis, with the problem picked up on abnormal liver function tests. However, they may present with:
- Abdominal pain in the right upper quadrant
- Pruritus (itching)
- Fatigue
- Jaundice
- Hepatomegaly
- Splenomegaly
Investigations
Liver function tests show:
- Raise alkaline phosphatase (the most notable liver enzyme as with most “obstructive” pathology)
- Other liver enzymes and bilirubin are raised later in the disease
Autoantibodies are not helpful in diagnosis or assessment. No antibodies are particularly sensitive or specific to primary sclerosing cholangitis. The main autoantibodies are:
- Perinuclear antineutrophil cytoplasmic antibody (p-ANCA)
- Antinuclear antibodies (ANA)
- Anti-smooth muscle antibodies (anti-SMA)
Magnetic resonance cholangiopancreatography (MRCP) is the diagnostic imaging investigation. It involves an MRI scan that gives a detailed view of the bile ducts, showing bile duct strictures in primary sclerosing cholangitis.
Colonoscopy should be performed to assess for ulcerative colitis.
Liver biopsy is not usually required but may be used where there is diagnostic uncertainty.
Management
There are no treatments proven to be effective for primary sclerosing cholangitis.
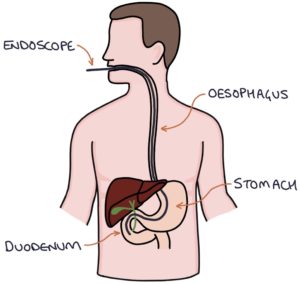
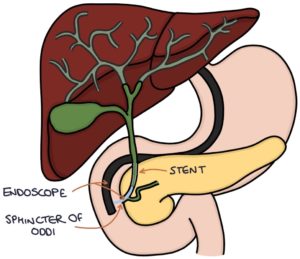
Endoscopic retrograde cholangio-pancreatography (ERCP) may be used to treat dominant strictures. This involves inserting an endoscope down the oesophagus, past the stomach, to the duodenum and the opening of the common bile duct (the sphincter of Oddi). This gives the operator access to the biliary system. Strictures can be dilated. Stents can be inserted to keep the ducts open. Antibiotics are given alongside ERCP to reduce the risk of infection (bacterial cholangitis).
Liver transplant is used in advanced disease, with around 80% survival at five years post-transplantation.
Other aspects of management include:
- Colestyramine for symptoms of pruritus (a bile acid sequestrant that reduces intestinal absorption of bile acids)
- Replacement of fat-soluble vitamins
- Monitoring for complications such as cholangiocarcinoma, cirrhosis and oesophageal varices
Complications
Complications and associations include:
- Biliary strictures
- Acute bacterial cholangitis
- Cholangiocarcinoma develops in 10-20% of cases
- Cirrhosis and the related complications (e.g., portal hypertension and oesophageal varices)
- Fat-soluble vitamin deficiency (A, D, E and K)
- Osteoporosis
- Colorectal cancer in patients with ulcerative colitis
TOM TIP: The association between ulcerative colitis, primary sclerosing cholangitis and cholangiocarcinoma is commonly tested in exams.
IgG4-Related Sclerosing Cholangitis
IgG4-related sclerosing cholangitis is similar to primary sclerosing cholangitis. Elevated IgG4 levels in the blood are the distinguishing feature. Unlikely primary sclerosing cholangitis, IgG4-related sclerosing cholangitis responds well to treatment with steroids. It is associated with autoimmune pancreatitis.
Last updated May 2023
Now, head over to members.zerotofinals.com and test your knowledge of this content. Testing yourself helps identify what you missed and strengthens your understanding and retention.

