Non-alcoholic fatty liver disease (NAFLD) is characterised by excessive fat in the liver cells, specifically triglycerides. These fat deposits interfere with the functioning of the liver cells. The early stages of NAFLD can be asymptomatic. However, it can progress to hepatitis and liver cirrhosis.
Around 25% of adults are estimated to have non-alcoholic fatty liver disease.
Stages
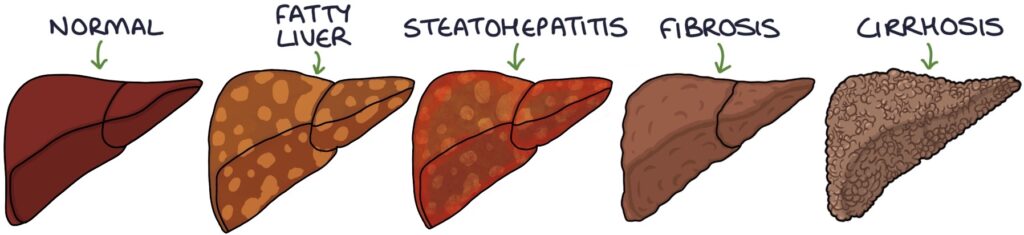
The stages of non-alcoholic fatty liver disease are:
- Non-alcoholic fatty liver disease
- Non-alcoholic steatohepatitis (NASH)
- Fibrosis
- Cirrhosis
Risk Factors
Non-alcoholic fatty liver disease shares the same risk factors as cardiovascular disease and diabetes:
- Middle age onwards
- Obesity
- Poor diet and low activity levels
- Type 2 diabetes
- High cholesterol
- High blood pressure
- Smoking
It is associated with metabolic syndrome, which is a combination of hypertension, obesity and diabetes. Metabolic syndrome is common and dramatically increases the risk of cardiovascular disease and other health problems.
Investigations
Raised alanine aminotransferase (ALT) on the liver function blood tests is often the first indication that a patient has NAFLD.
Liver ultrasound can confirm the diagnosis of hepatic steatosis (fatty liver), seen as increased echogenicity. Ultrasound does not indicate the severity, function of the liver or presence of fibrosis. It can be normal in NAFLD.
The enhanced liver fibrosis (ELF) blood test is the first-line investigation for assessing fibrosis in non-alcoholic fatty liver disease. It measures three markers (HA, PIIINP and TIMP-1) and uses an algorithm to provide a result that indicates whether they have advanced fibrosis of the liver:
- 10.51 or above – advanced fibrosis
- Under 10.51 – unlikely advanced fibrosis (NICE recommend rechecking every 3 years in NAFLD)
NAFLD Fibrosis Score (NFS) is another option for assessing liver fibrosis in NAFLD. It is based on an algorithm of age, BMI, liver enzymes (AST and ALT), platelet count, albumin and diabetes.
Fibrosis 4 (FIB-4) score is another option for assessing liver fibrosis in NAFLD. It is based on an algorithm of age, liver enzymes (AST and ALT) and platelet count.
Transient elastography (“FibroScan”) can be used to assess the stiffness of the liver using high-frequency sound waves. It helps determine the degree of fibrosis (scarring) to test for liver cirrhosis. It is used where the enhanced liver fibrosis (ELF) test indicates advanced fibrosis.
Liver biopsy may be required to confirm the diagnosis and exclude other causes of liver disease.
TOM TIP: Both the NFS and FIB-4 scores use the AST:ALT ratio to assess the severity of liver fibrosis. The normal ratio is less than 1. A ratio greater than 0.8 in NAFLD suggests advanced fibrosis. An AST:ALT ratio greater than 1.5 (meaning a disproportionately high AST) indicates alcohol-related liver disease rather than NAFLD.
Diagnosis
The diagnosis requires the presence of ultrasound findings of a fatty liver, risk factors and excluding other causes of liver disease with a careful alcohol history and full non-invasive liver screen. Liver biopsy is the gold standard test.
Management
Management involves:
- Weight loss
- Healthy diet (Mediterranean diet is recommended)
- Exercise
- Avoid/limit alcohol intake
- Stop smoking
- Control of diabetes, blood pressure and cholesterol
- Refer patients where scoring tests indicate liver fibrosis to a liver specialist
- Specialist management may include vitamin E, pioglitazone, bariatric surgery and liver transplantation
Last updated May 2023
Now, head over to members.zerotofinals.com and test your knowledge of this content. Testing yourself helps identify what you missed and strengthens your understanding and retention.

