An entire liver can be transplanted from a deceased donor to a recipient.
The liver has the ability to regenerate. It is possible to take a portion of the liver from a living donor, transplant it into a patient and have both regenerate to become two fully functioning organs. This is known as a living donor transplant.
It is also possible to split the liver of a deceased person into two and transplant the two parts into two patients and have them regenerate to function normally in both recipients. This is known as a split donation.
When the patient’s diseased liver is removed and the new liver placed in the same anatomical location, it is known as an orthotopic transplant. This translates as straight (ortho-) in place (-topic). This is in contrast to a heterotopic transplant, which involves adding the new organ away from the existing organs (e.g., adding a transplanted kidney in the lower abdomen without removing the native kidneys during a kidney transplant).
Indications
Indications for liver transplants fall into two categories: acute liver failure and chronic liver failure. They may also be used in specific cases of hepatocellular carcinoma.
Acute liver failure usually requires an immediate liver transplant, and these patients are placed at the top of the list. The most common causes are acute viral hepatitis and paracetamol overdose.
Chronic liver failure patients can wait longer for their liver transplant and are put on a standard transplant list. It is usual for it to take around 5 months for a liver to become available.
Suitability for Liver Transplantation
The British Society of Gastroenterologists provides guidelines on liver transplantation (2019), including when to refer and the contraindications.
Contraindications include:
- Significant co-morbidities (e.g., severe kidney, lung or heart disease)
- Current illicit drug use
- Continuing alcohol misuse (generally 6 months of abstinence is required)
- Untreated HIV
- Current or previous cancer (except certain liver cancers)
Surgery
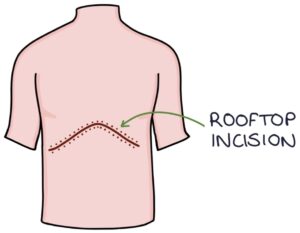
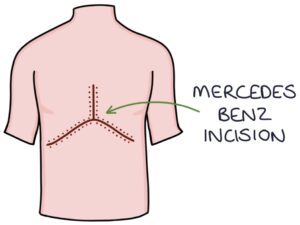
The liver transplant surgery is carried out in a specialist transplant centre. It involves a “rooftop” or “Mercedes Benz” incision along the lower costal margin for open surgery. The liver is mobilised away from the other tissues and excised.
When an entire donor liver is implanted, the donor liver’s inferior vena cava, hepatic artery, portal vein and common bile duct are anastomosed with the recipient’s.
With a split donation, the remaining branches of the donated portion of liver are anastomosed with the recipient. For example, with a left lobe liver transplantation, the left hepatic vein, left hepatic artery, left portal vein and left hepatic duct are anastomosed with the recipient’s inferior vena cava, hepatic artery, portal vein and common bile duct.
Post-Transplantation Care
Patients will require lifelong immunosuppression (e.g., steroids, azathioprine and tacrolimus) and careful monitoring of these drugs. They are required to follow lifestyle advice and require monitoring and treatment for complications:
- Avoid alcohol and smoking
- Treating opportunistic infections
- Monitoring for disease recurrence (e.g., autoimmune hepatitis or primary biliary cholangitis)
- Monitoring for cancer, as there is a significantly higher risk in immunosuppressed patients
Monitoring for evidence of transplant rejection:
- Abnormal LFTs
- Fatigue
- Fever
- Jaundice
Last updated May 2023
Now, head over to members.zerotofinals.com and test your knowledge of this content. Testing yourself helps identify what you missed and strengthens your understanding and retention.

