Inflammatory bowel disease involves recurrent episodes of inflammation in the gastrointestinal tract. The two main types are ulcerative colitis and Crohn’s disease. They are associated with periods of exacerbation and remission.
Inflammatory bowel disease is thought to be caused by a combination of factors related to genetics, environment and the gut microbiome. The typical patient presents in their 20s.
Features
The general presenting features of inflammatory bowel disease are:
- Diarrhoea
- Abdominal pain
- Rectal bleeding
- Fatigue
- Weight loss
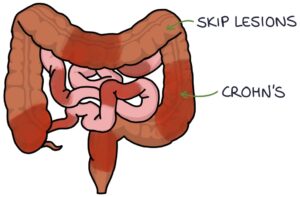
Differentiating features of Crohn’s can be remembered with the “crows” NESTS mnemonic:
- N – No blood or mucus (PR bleeding is less common)
- E – Entire gastrointestinal tract affected (from mouth to anus)
- S – “Skip lesions” on endoscopy
- T – Terminal ileum most affected and Transmural (full thickness) inflammation
- S – Smoking is a risk factor (don’t set the nest on fire)
Crohn’s is also associated with strictures and fistulas.
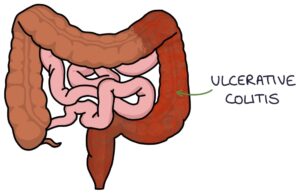
Differentiating features of ulcerative colitis can be remembered with the “you see (UC)” CLOSEUP mnemonic:
- C – Continuous inflammation
- L – Limited to the colon and rectum
- O – Only superficial mucosa affected
- S – Smoking may be protective (ulcerative colitis is less common in smokers)
- E – Excrete blood and mucus
- U – Use aminosalicylates
- P – Primary sclerosing cholangitis
TOM TIP: It is common for exams to give you some features and ask you to determine whether the patient has Crohn’s or ulcerative colitis. This might be a finding of skip lesions on an endoscopy, transmural inflammation or mouth ulcers to suggest Crohn’s rather than ulcerative colitis.
Associations
Many associated conditions can occur in patients with inflammatory bowel disease:
- Erythema nodosum (tender, red nodules on the shins caused by inflammation of the subcutaneous fat)
- Pyoderma gangrenosum (rapidly enlarging, painful skin ulcers)
- Enteropathic arthritis (a type of inflammatory arthritis)
- Primary sclerosing cholangitis (particularly with ulcerative colitis)
- Red eye conditions (e.g., episcleritis, scleritis and anterior uveitis)
Investigations
Blood tests include:
- Full blood count for haemoglobin (low in anaemia) and platelet count (raised with inflammation)
- C-reactive protein (CRP) indicates inflammation
- Urea and electrolytes (U&Es) indicate electrolyte imbalances and kidney function
- Liver function tests (LFTs) can show low albumin in severe disease (protein is lost in the bowel)
- Thyroid function tests for hyperthyroidism as a cause of diarrhoea
- Anti-tissue transglutaminase antibodies (anti-TTG) for coeliac disease as a differential diagnosis
Stool microscopy and culture can be used to exclude infection as a differential diagnosis (e.g., Salmonella).
Faecal calprotectin is around 90% sensitive and specific for inflammatory bowel disease in adults. It is used as an initial test before moving on to endoscopy.
Colonoscopy with multiple intestinal biopsies is the investigation of choice for establishing the diagnosis.
Imaging investigations (e.g., ultrasound, CT and MRI) can be used to look for complications such as fistulas, abscesses and strictures.
Management
Management of inflammatory bowel disease can be separated into:
- Inducing remission during an acute exacerbation
- Maintaining remission
Systemically unwell patients require hospital admission.
Patients should be under the care of a gastroenterologist, with support from specialist nurses.
Ulcerative Colitis Management
Mild to moderate acute ulcerative colitis is treated with:
- Aminosalicylate (e.g., oral or rectal mesalazine) first-line
- Corticosteroids (e.g., oral or rectal prednisolone) second-line
Severe acute ulcerative colitis is treated with:
- Intravenous steroids (e.g., IV hydrocortisone) first-line
Other options for severe acute ulcerative colitis include:
- Intravenous ciclosporin
- Infliximab
- Surgery
Options for maintaining remission in ulcerative colitis are:
- Aminosalicylate (e.g., oral or rectal mesalazine) first-line
- Azathioprine
- Mercaptopurine
Ulcerative colitis typically only affects the large bowel and rectum. Therefore, removing the entire large bowel and rectum (panproctocolectomy) will remove the disease. The patient has either a permanent ileostomy or an ileo-anal anastomosis (J-pouch).
An ileostomy is where the end portion of the small bowel (ileum) is brought onto the skin with a spout that drains stools directly into a tightly fitting stoma bag.
A J-pouch is where the ileum (small bowel) is folded back on itself and fashioned into a larger pouch, which is attached to the anus and functions like a rectum, collecting stools before the person opens their bowels.
Crohn’s Management
Inducing remission in an exacerbation of Crohn’s disease is with:
- Steroids (e.g., oral prednisolone or IV hydrocortisone) first-line
- Enteral nutrition as an alternative, particularly where there are concerns about steroids affecting growth
Enteral nutrition involves a specially formulated liquid diet given orally or by NG feed that replaces the patient’s diet. This induces remission by:
- Treating nutritional deficiencies
- Improving the gut microbiome
- Removing inflammatory foods
Where steroids alone are inadequate, adding other medications may be considered:
- Azathioprine
- Mercaptopurine
- Methotrexate
- Infliximab
- Adalimumab
Maintaining remission in Crohn’s disease is tailored to the individual, based on risks, side effects, nature of the disease and patient wishes. This might involve no medications.
First-line for maintaining remission in Crohn’s is with either:
- Azathioprine
- Mercaptopurine
Methotrexate is an alternative for maintaining remission where first-line options are unsuitable.
Surgical options for Crohn’s include:
- Resecting the distal ileum when the disease is isolated to this area
- Treating strictures
- Treating fistulas
Last updated May 2023
Now, head over to members.zerotofinals.com and test your knowledge of this content. Testing yourself helps identify what you missed and strengthens your understanding and retention.

