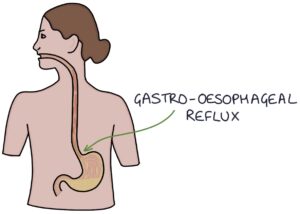
Gastro-oesophageal reflux disease (GORD) is where acid from the stomach flows through the lower oesophageal sphincter and into the oesophagus, where it irritates the lining and causes symptoms.
The oesophagus has a squamous epithelial lining that makes it more sensitive to the effects of stomach acid. The stomach has a columnar epithelial lining that is more protected against stomach acid.
Causes and Triggers
Certain factors can exacerbate or worsen the symptoms of GORD:
- Greasy and spicy foods
- Coffee and tea
- Alcohol
- Non-steroidal anti-inflammatory drugs
- Stress
- Smoking
- Obesity
- Hiatus hernia
Presentation
Dyspepsia is a non-specific term used to describe indigestion. It covers the symptoms of GORD:
- Heartburn
- Acid regurgitation
- Retrosternal or epigastric pain
- Bloating
- Nocturnal cough
- Hoarse voice
Red Flags
Patients with symptoms suspicious of cancer get a two week wait referral for further investigation. It is possible to refer from primary care for an urgent direct-access endoscopy. The NICE guidelines on suspected cancer (2021) have criteria for when to refer urgently or routinely.
The key red flag features are:
- Dysphagia (difficulty swallowing) at any age gets an immediate two week wait referral
- Aged over 55 (this is generally the cut-off for urgent versus routine referrals)
- Weight loss
- Upper abdominal pain
- Reflux
- Treatment-resistant dyspepsia
- Nausea and vomiting
- Upper abdominal mass on palpation
- Low haemoglobin (anaemia)
- Raised platelet count
TOM TIP: Remember dysphagia as a critical red flag. Any patient presenting with the feeling that food is getting stuck on the way down needs an urgent two week wait referral for an endoscopy.
Endoscopy
An oesophago-gastro-duodenoscopy (OGD) involves inserting a camera through the mouth down to the oesophagus, stomach and duodenum. It can be used to assess for:
- Gastritis
- Peptic ulcers
- Upper gastrointestinal bleeding
- Oesophageal varices (in liver cirrhosis)
- Barretts oesophagus
- Oesophageal stricture
- Malignancy of the oesophagus or stomach
Patients with evidence of upper gastrointestinal bleeding (e.g., melaena or coffee ground vomiting) need admission and urgent endoscopy.
Hiatus Hernias
A hiatus hernia refers to the herniation of the stomach up through the diaphragm. The diaphragm opening should be at the lower oesophageal sphincter level and fixed in place. A narrow opening helps to maintain the sphincter and stops acid and stomach contents from refluxing into the oesophagus. When the opening of the diaphragm is wider, the stomach can enter through the diaphragm, and the contents of the stomach can reflux into the oesophagus.
There are four types of hiatus hernia:
- Type 1: Sliding
- Type 2: Rolling
- Type 3: Combination of sliding and rolling
- Type 4: Large opening with additional abdominal organs entering the thorax
A sliding hiatus hernia is where the stomach slides up through the diaphragm, with the gastro-oesophageal junction passing up into the thorax.
A rolling hiatus hernia is where a separate portion of the stomach (i.e., the fundus), folds around and enters through the diaphragm opening, alongside the oesophagus.
Type 4 hiatus hernia refers to a large hernia that allows other intra-abdominal organs to pass through the diaphragm opening (e.g., bowel, pancreas or omentum).
Hiatus hernias can be intermittent, meaning they may not be seen on investigations. Hiatus hernias may be seen on a:
- Chest x-ray
- CT scan
- Endoscopy
- Barium swallow test
Management
Management of gastro-oesophageal reflux disease can be split into:
- Lifestyle changes
- Reviewing medications (e.g., stop NSAIDs)
- Antacids (e.g., Gaviscon, Pepto-Bismol and Rennie) – short term only
- Proton pump inhibitors (e.g., omeprazole and lansoprazole)
- Histamine H2-receptor antagonists (e.g., famotidine)
- Surgery
Lifestyle changes include:
- Reduce tea, coffee and alcohol
- Weight loss
- Avoid smoking
- Smaller, lighter meals
- Avoid heavy meals before bedtime
- Stay upright after meals rather than lying flat
Surgery for reflux is called laparoscopic fundoplication. This involves tying the fundus of the stomach around the lower oesophagus to narrow the lower oesophageal sphincter.
TOM TIP: The usual medical strategy when someone presents for the first time is to exclude red flags, address potential triggers, offer a 1 month trial of a proton pump inhibitor and consider H. pylori testing.
Helicobacter Pylori
Helicobacter pylori (H. pylori) is a gram-negative aerobic bacteria that can live in the stomach. It causes damage to the epithelial lining, resulting in gastritis, ulcers and an increased risk of stomach cancer. It avoids the acidic environment by forcing its way into the gastric mucosa, using flagella to propel itself. It creates gaps in the mucosa, exposing the epithelial cells underneath to damage from stomach acid.
H. pylori produces ammonium hydroxide, which neutralises the acid surrounding the bacteria. It also produces several toxins. The ammonia and toxins lead to gastric mucosal damage.
We offer a test for H. pylori to anyone with dyspepsia. They need 2 weeks without using a PPI before testing for H. pylori for an accurate result.
Investigations for H. Pylori are:
- Stool antigen test
- Urea breath test using radiolabelled carbon 13
- H. pylori antibody test (blood)
- Rapid urease test performed during endoscopy (also known as the CLO test)
A rapid urease test involves taking a small biopsy of the stomach mucosa. This is added to a liquid medium containing urea. H. pylori produce urease enzymes that convert urea to ammonia. Ammonia makes the solution more alkaline. A pH indicator (e.g., phenol red) changes colour if the pH rises, giving a positive result.
The H. pylori eradication regime involves triple therapy with a proton pump inhibitor (e.g., omeprazole) plus two antibiotics (e.g., amoxicillin and clarithromycin) for 7 days. Routine re-testing is not necessary after treatment.
Barrett’s Oesophagus
Barrett’s oesophagus refers to when the lower oesophageal epithelium changes from squamous to columnar epithelium. This process is called metaplasia. It is caused by chronic acid reflux into the oesophagus. Patients may notice improved reflux symptoms after they develop Barrett’s oesophagus.
Barrett’s oesophagus is a premalignant condition and a significant risk factor for developing oesophageal adenocarcinoma (cancer of the epithelial cells). There can be a stepwise progression from no dysplasia to low-grade dysplasia, high-grade dysphasia, and adenocarcinoma.
Treatment of Barrett’s oesophagus is with:
- Endoscopic monitoring for progression to adenocarcinoma
- Proton pump inhibitors
- Endoscopic ablation (e.g., radiofrequency ablation)
Ablation can be used to destroy abnormal columnar epithelial cells, which are then replaced with normal squamous epithelial cells. Ablation has a role in treating low and high-grade dysplasia to reduce cancer risk.
TOM TIP: The histology of Barrett’s oesophagus is a common exam topic. Remember the term metaplasia, which means a change in the type of cell. This is different from dysplasia, which refers to the presence of abnormal cells. Remember that the normal epithelium is squamous, and in Barrett’s it changes to columnar.
Zollinger–Ellison Syndrome
Zollinger-Ellison syndrome is a rare condition where a duodenal or pancreatic tumour secretes excessive quantities of gastrin. Gastrin is a hormone that stimulates acid secretion in the stomach. Therefore, there is excess production of stomach acid, resulting in severe dyspepsia, diarrhoea and peptic ulcers.
Gastrin-secreting tumours (gastrinomas) may be associated with multiple endocrine neoplasia type 1 (MEN1), an autosomal dominant genetic condition, which can also cause hormone-secreting tumours of the parathyroid and pituitary glands.
Last updated May 2023
Now, head over to members.zerotofinals.com and test your knowledge of this content. Testing yourself helps identify what you missed and strengthens your understanding and retention.

