Alpha-1 antitrypsin deficiency is a genetic condition caused by low levels of alpha-1 antitrypsin.
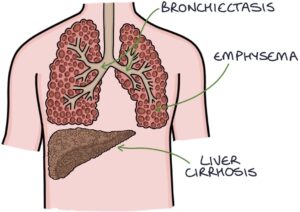
Two main organs are affected by alpha-1 antitrypsin deficiency:
- Chronic obstructive pulmonary disease and bronchiectasis in the lungs (typically after 30 years old)
- Dysfunction, fibrosis and cirrhosis of the liver (depending on the specific genotype)
Pathophysiology
The SERPINA1 gene coding for alpha-1 antitrypsin is found on chromosome 14. The gene has many potential variations, each with different effects on the quantity and functionality of alpha-1 antitrypsin.
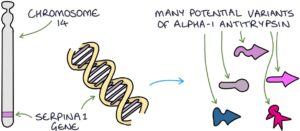
Alpha-1 antitrypsin deficiency is inherited in an autosomal co-dominant pattern. Co-dominant refers to when both gene copies are expressed and contribute to the outcome (neither is dominant or recessive over the other). The disease severity results from the combination of both copies of the gene.
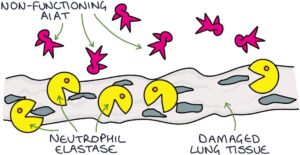
Alpha-1 antitrypsin is a protease inhibitor. One critical protease enzyme is neutrophil elastase. This enzyme, secreted by neutrophils, digests elastin (elastolysis), a protein in connective tissue that helps keep the tissues flexible. Alpha-1 antitrypsin (AAT) offers protection by inhibiting the action of neutrophil elastase.
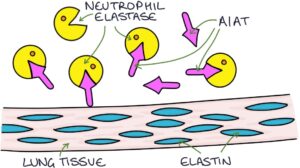
In the lungs, the lack of a normal, functioning alpha-1 antitrypsin protein leads to excess protease enzymes attacking the connective tissues. Destruction of elastic tissue in the lungs leads to bronchiectasis and emphysema. Smoking dramatically accelerates this process.
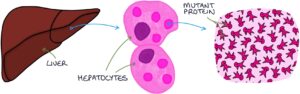
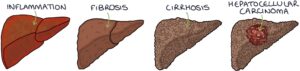
Alpha-1 antitrypsin is produced in the liver. In specific genotypes of alpha-1 antitrypsin deficiency, an abnormal mutant version of the protein is made that gets trapped and builds up inside the liver cells (hepatocytes). These mutant proteins are toxic to the hepatocytes, causing inflammation. Over time this progresses to fibrosis, cirrhosis and potentially hepatocellular carcinoma. Liver pathology can occur at any age, including childhood.
Less commonly, it can be associated with:
- Panniculitis (tender skin nodules caused by inflammation of the subcutaneous fat)
- Granulomatosis with polyangiitis (a small and medium vessel vasculitis)
Diagnosis
Diagnosis is based on:
- Low serum alpha-1 antitrypsin (the screening test)
- Genetic testing
Lung damage is assessed with:
- Chest x-ray
- High-resolution CT thorax
- Pulmonary function tests
Liver biopsy shows periodic acid-Schiff positive staining globules in hepatocytes, resistant to diastase treatment. These represent a buildup of the mutant proteins.
Management
Management involves:
- Stop smoking
- Symptomatic management (e.g., standard treatment of COPD)
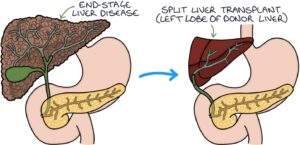
- Organ transplant for end-stage liver or lung disease
- Monitoring for complications (e.g., hepatocellular carcinoma)
- Screening of family members
Giving an infusion of alpha-1 antitrypsin to boost the levels is possible, but there is doubt about the clinical benefit and cost. The NICE guidelines on COPD (updated 2019) recommend against using replacement alpha-1 antitrypsin.
Last updated May 2023
Now, head over to members.zerotofinals.com and test your knowledge of this content. Testing yourself helps identify what you missed and strengthens your understanding and retention.